Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 | |
 |  |
 |  |
 |  |
 | /Buspar-59434dcd5f9b58d58a0b0b94.jpg) |
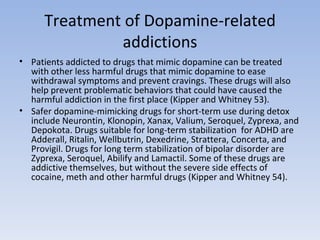
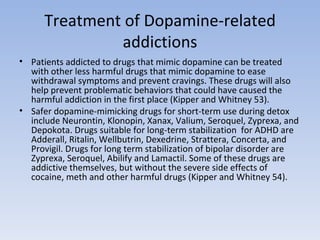
Key takeaways Gabapentin is not FDA approved for bipolar disorder, and studies show limited evidence of its effectiveness for this purpose. While it may help with symptoms like anxiety and insomnia, gabapentin’s benefits for bipolar disorder are inconclusive. Gabapentin can cause side effects such as drowsiness and dizziness and may interact with other medications. Gabapentin dosages for The use of gabapentin in bipolar disorder (BPD) treatment provides an informative case of off-label uptake and abandonment of a new medication. Gabapentin was patented by Warner-Lambert in 1977 and FDA-approved in December1993 for the adjunctive treatment of epilepsy and in 2002 for postherpetic neuralgia (see Appendix 1 for timeline). The drugs gabapentin and pregabalin are sometimes prescribed for people with bipolar disorder or insomnia. Research found little evidence that they are effective. The drugs have side effects and can be addictive; the team calls for further trials. Gabapentin and pregabalin (collectively known as gabapentinoids) are licensed in the UK to treat pain and seizures. Despite its prevalence and disease burden, several chasms still exist with regard to the pharmacotherapy of bipolar disorder (BD). Polypharmacy is commonly encountered as a significant proportion of patients remain symptomatic, and the management of the depressive phase of the illness is a particular challenge. Gabapentin and pregabalin have often been prescribed off-label in spite of a Key takeaways: Gabapentin is a medication that’s used to treat seizures, nerve pain from shingles, and restless leg syndrome. Despite previous marketing claims, there’s no evidence that gabapentin is a good treatment for bipolar disorder. The best treatment for bipolar disorder is therapy and a combination of other medications. These include mood stabilizers, anticonvulsants, and From the data presented, gabapentin cannot be recommended for treatment of bipolar disorder. Further studies are required to determine whether gabapentin has any role in the management of bipolar disorder. Gabapentin is a nerve pain medication and anticonvulsant that has proven to be effective for people who have hard-to-treat depression or other mood disorders. Gabapentin may be a useful drug for the add-on treatment of bipolar patients with poor response to other mood stabilizers. Gabapentin may improve depressive residual symptoms such as irritability, social withdrawal or anxiety. These results should be confirmed in randomized clinical trials. Two new anticonvulsants, lamotrigine and gabapentin, have been used increasingly for bipolar disorder in the past several years. Despite this array of options, bipolar disorder remains a difficult disorder to treat. Some subtypes, such as those characterized by rapid cycling or mixed episodes, have been especially resistant to lithium treatment. Prescribing-Based Evidence To facilitate learning, I have at-tached whimsical names to all the pru-dent options available to the prescriber to treat bipolar spectrum disorders while the experts clarify the data and remove the controversy (Table 1). Anticonvulsants: Perhaps one of the reasons so many anticonvulsants that are not well documented to have efficacy in bipolar disorder are never Results Evidence supports gabapentin as a treatment for alcohol withdrawal and alcohol use disorder. There is sufficient evidence to consider gabapentin as a third-line treatment for social anxiety disorder and severe panic disorder. Systematic reviews of gabapentin treatment in psychiatric and/or substance use disorders showed inconclusive evidence for efficacy in BD, but possible efficacy for some anxiety disorders [9, 10]. Gabapentin is commonly used off-label in the treatment of psychiatric disorders with success, failure, and controversy. A systematic review of the literature was performed to elucidate the evidence for clinical benefit of gabapentin in psychiatric The gabapentinoids, gabapentin, and pregabalin, target the α<sub>2</sub>δ subunits of voltage-gated calcium channels. Initially licensed for pain and seizures, they have become widely prescribed drugs. Many of these uses are off-label for psychiatric indications, and there is increasing concern abou Abstract Background: Gabapentin, a new anti-epileptic agent, has been anecdotally reported to be effective in the treatment of mania. We systematically assessed the response rate in bipolar patients being treated adjunctively with gabapentin for manic symptoms, depressive symptoms, or rapid cycling not responsive to standard treatments. Unfortunately, gabapentin does not demonstrate efficacy in randomized trials for bipolar disorder and current treatment guidelines do not emphasize its use. Despite of the lack of evidence, reviews of gabapentin prescribing patterns in the United States show that this medication is still being used with alarming frequency for bipolar disorder. Results: Gabapentin was moderately to mark-edly effective in 30% (15/50) of patients, with statistically nonsignificant differences between patients with bipolar disorder type I, bipolar dis-order type II and NOS, and unipolar major de-pressive disorder. 70% reported side effects, mainly sedation, with 16% of the total sample discontinuing treatment due to adverse events. Conclusion Using Gabapentin as a Treatment Option In recent years, gabapentin has been studied as a potential adjunctive treatment for bipolar disorder. Studies have shown that gabapentin can help reduce symptoms of depression and anxiety in patients with bipolar disorder, particularly when used in conjunction with other medications. Abstract Despite its prevalence and disease burden, several chasms still exist with regard to the pharmacotherapy of bipolar disorder (BD). Polypharmacy is commonly encountered as a significant proportion of patients remain symptomatic, and the management of the depressive phase of the illness is a particular challenge. Gabapentin and pregabalin have often been prescribed off-label in spite of Secondary outcomes Secondary outcomes included the acceptability and tolerability of gabapentin or pregabalin in acute/long-term treatment of BD, anxiety, and insomnia.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 | |
 |  |
 |  |
 |  |
 | /Buspar-59434dcd5f9b58d58a0b0b94.jpg) |