Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |
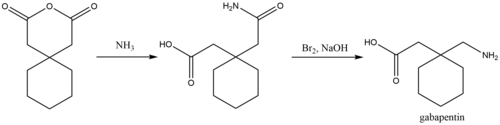
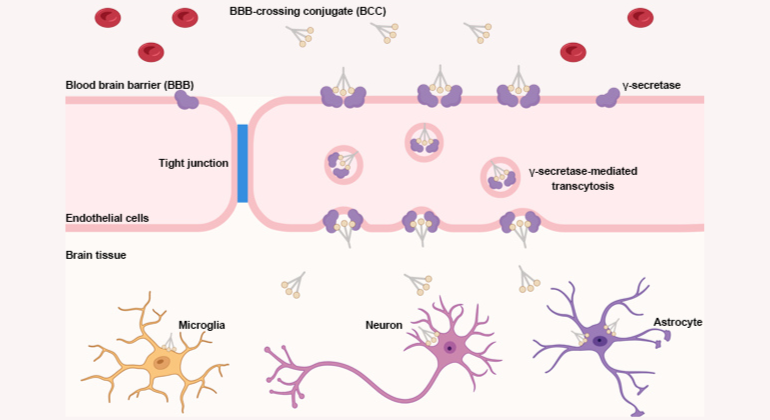
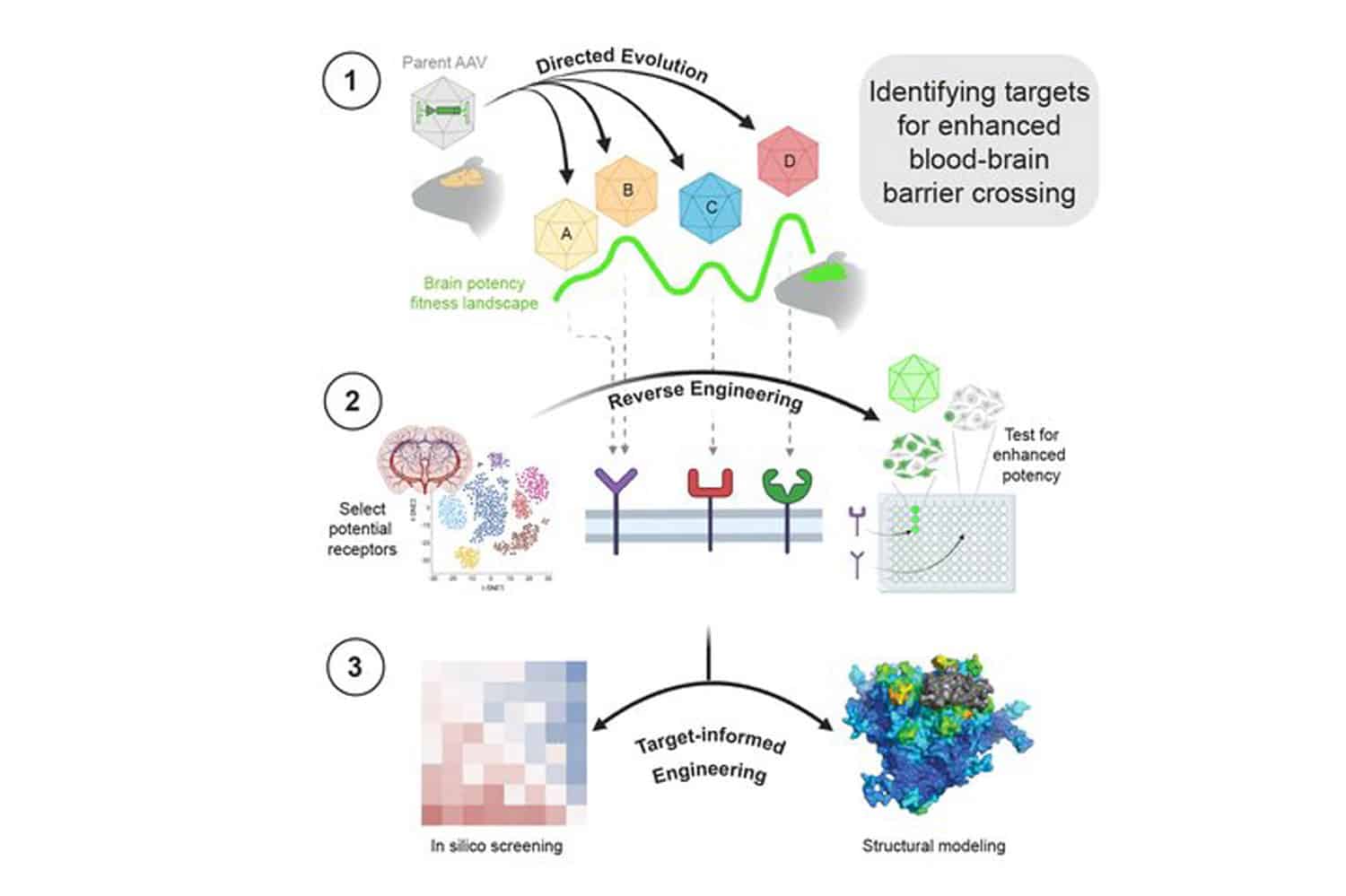
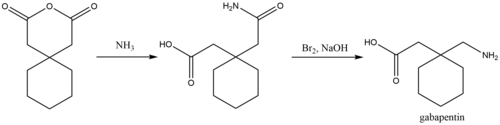
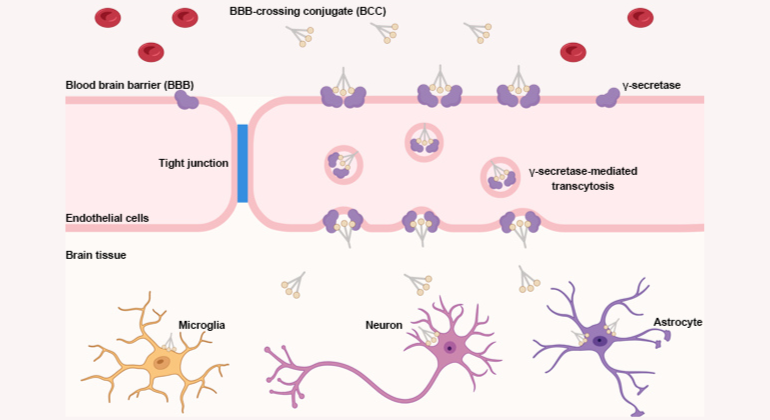
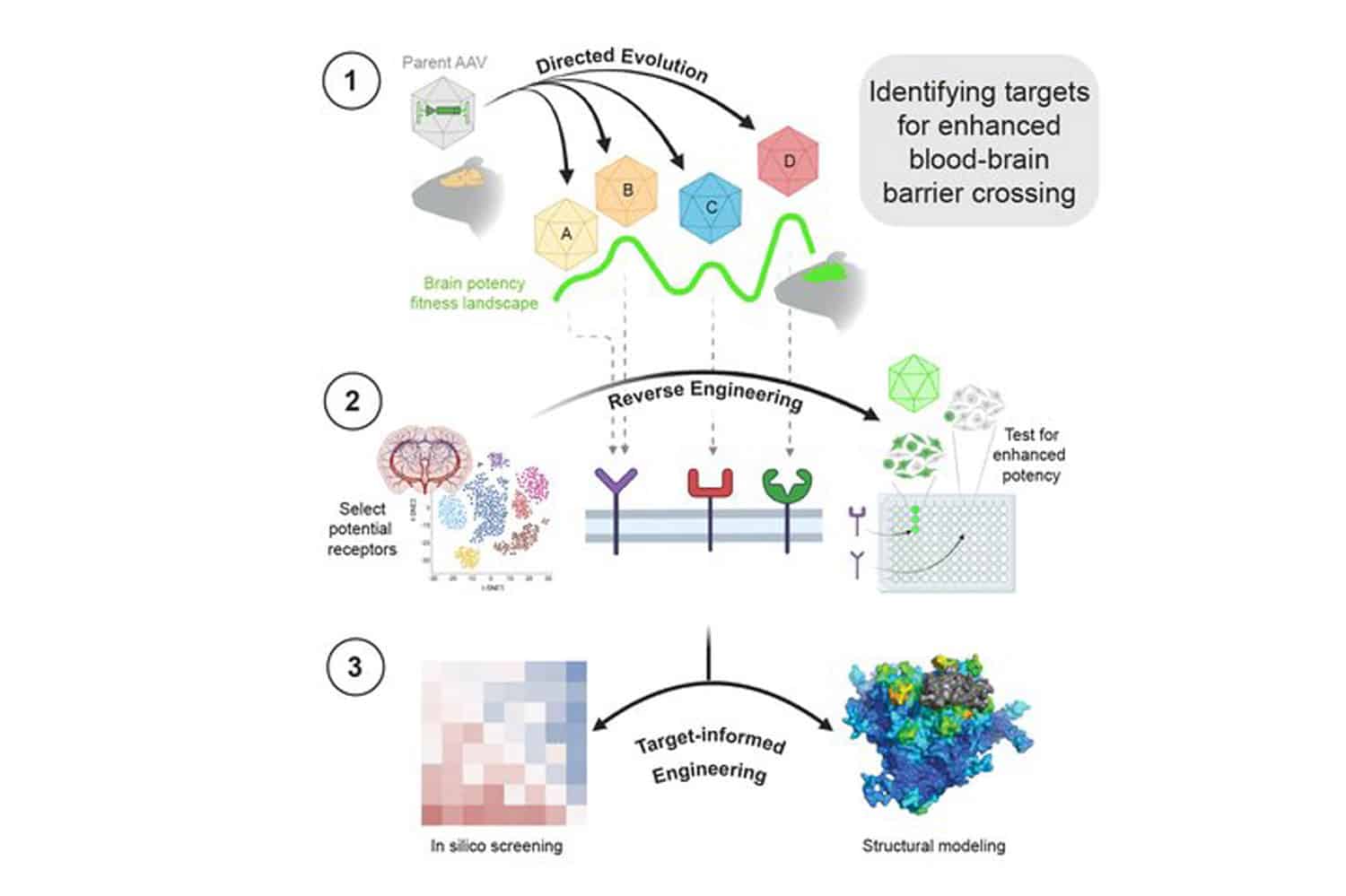
Although the exact mechanism of action with the GABA receptors is unknown, researchers know that gabapentin freely passes the blood-brain barrier and acts on neurotransmitters. Prescription GABA Derivitives Because of its importance as a neurotransmitter, pharmaceutical manufacturers have worked to design prescription GABA analogues that can cross the blood-brain barrier and mimic GABA. Gabapentin is a GABA analogue used to treat epilepsy and neurotic pain. Gabapentin causes an increase in GABA levels in the brain. MeSH terms Amines / pharmacokinetics* Biological Transport Blood-Brain Barrier Blotting, Western Brain / blood supply Brain / metabolism Cell Line Cyclohexanecarboxylic Acids / pharmacokinetics* Gabapentin Humans Large Neutral Amino Acid-Transporter 1 / physiology* Reverse Transcriptase Polymerase Chain Reaction gamma-Aminobutyric Acid Blood–Brain Barrier Permeability The BBB protects most of the brain from toxins and ion abnormalities that find their way into vascular space through ingestion, infection, or other means (Purves et al., 2004). On the one hand, the BBB is important in keeping the brain safe from harmful substances. Gabapentin was originally designed as an anticonvulsant γ-aminobutyric acid (GABA) mimetic capable of crossing the blood-brain barrier. In the present review we show that although gabapentin is not a GABA mimetic, it has great utility as an add-on therapy for epilepsy and as a first-line treatment for neuropathic pain. Although gabapentin is not considered highly addictive, it does cross the blood-brain barrier and has a risk for physical dependence. Treating Brain Damage with Gabapentin Gabapentin can be an effective treatment for brain damage symptoms such as neuropathy, seizures, and autonomic dysfunction. However, it is not without side effects or risks. Gabapentin crosses the blood–brain barrier more easily than GABA. In the early patents, the Goedecke researchers noted that the compound is a sedative; and in mice, it prevented seizures triggered by a GABA antagonist. Preliminary clinical trials in the 1980s indicated that gabapentin appeared to be effective against spasticity and migraines. Take-home message: - gamma-Aminobutyric acid (GABA) is a major neurotransmitter that regulates much of our brain function. It was previously thought that ingested GABA could not cross the blood-brain barrier, but new research suggests that it may be able to. - Drugs that mimic the action of GABA are numerous, work in a variety of ways, and can have effects ranging from treating epilepsy to As gabapentin acts in the brain, the blood–brain barrier (BBB) will be important in regulating drug penetration. Gabapentin can readily cross the BBB, but the blood and brain concentrations are not proportional to dose [9]. The passage of gabapentin across the BBB has been shown to be saturable [10]. Gabapentin can cross the blood–brain barrier and enter the central nervous system. [89] Gabapentin concentration in cerebrospinal fluid is approximately 9–14% of its blood plasma concentration. [98] Although it is rapidly absorbed, readily crosses the blood–brain barrier and is orally active in several animal models of epilepsy, gabapentin neither binds to GABA A or GABA B receptors nor is it metabolized to GABA (Goa and Sorkin, 1993; Kammerer et al, 2011; Taylor et al, 1992). Gabapentin, a GABA analog since 1993, crosses the blood-brain barrier, binds α₂δ calcium channels, has dose-dependent absorption, renal clearance, and may cause dizziness and fatigue. Gabapentin, marketed for the treatment of seizures and neuropathic pain, has been shown to increase in vivo GABA concentration in the brain of both rodents and humans. Blood-brain barrier saturation of gabapentin transport was evident as the AUCratio decreased with increased AUCplasma. Collectively, these results support a trend towards saturation at higher plasma concentrations of the carrier-mediated transport mechanism of gabapentin through the blood-brain barrier. Although gabapentin is a structural analogue of the neurotransmitter gamma-aminobutyric acid (GABA), which does not cross the blood-brain barrier, gabapentin penetrates into the CNS and its activity is seemingly distinct from GABA-related effects. Lipophilic groups were added to the carbon backbone to increase the bioavailability of GABA, as it does not penetrate the blood–brain barrier. 8 This led to the serendipitous discovery of gabapentin as a potent anticonvulsant. The development of pregabalin was similarly fortuitous. Although gabapentin is a structural analogue of the neurotransmitter γ-aminobutyric acid (GABA), which does not cross the blood-brain barrier, gabapentin penetrates into the CNS and its activity is seemingly distinct from GABA-related effects. Blood-brain barrier saturation of gabapentin transport was evident as the AUC ratio decreased with increased AUC piasma. Collectively, these results support a trend towards saturation at higher plasma concentrations of the carrier-mediated transport mechanism of gabapentin through the blood-brain barrier. The blood–brain barrier (BBB) prevents the brain uptake of most pharmaceuticals. This property arises from the epithelial-like tight junctions within the brain capillary endothelium. The BBB is anatomically and functionally distinct from the Purpose. To determine the apparent bidirectional permeabilities of gabapentin (GBP) across the blood-brain barrier (BBB) using a novel microdialysis-pharmacokinetic approach. Methods. Rats were administered intravenous infusions of [14C]GBP to achieve clinically relevant steady-state plasma concentrations. Microdialysis was used to monitor GBP concentration in brain extracellular fluid (ECF
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |