Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
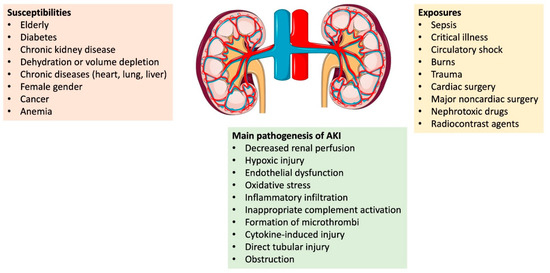
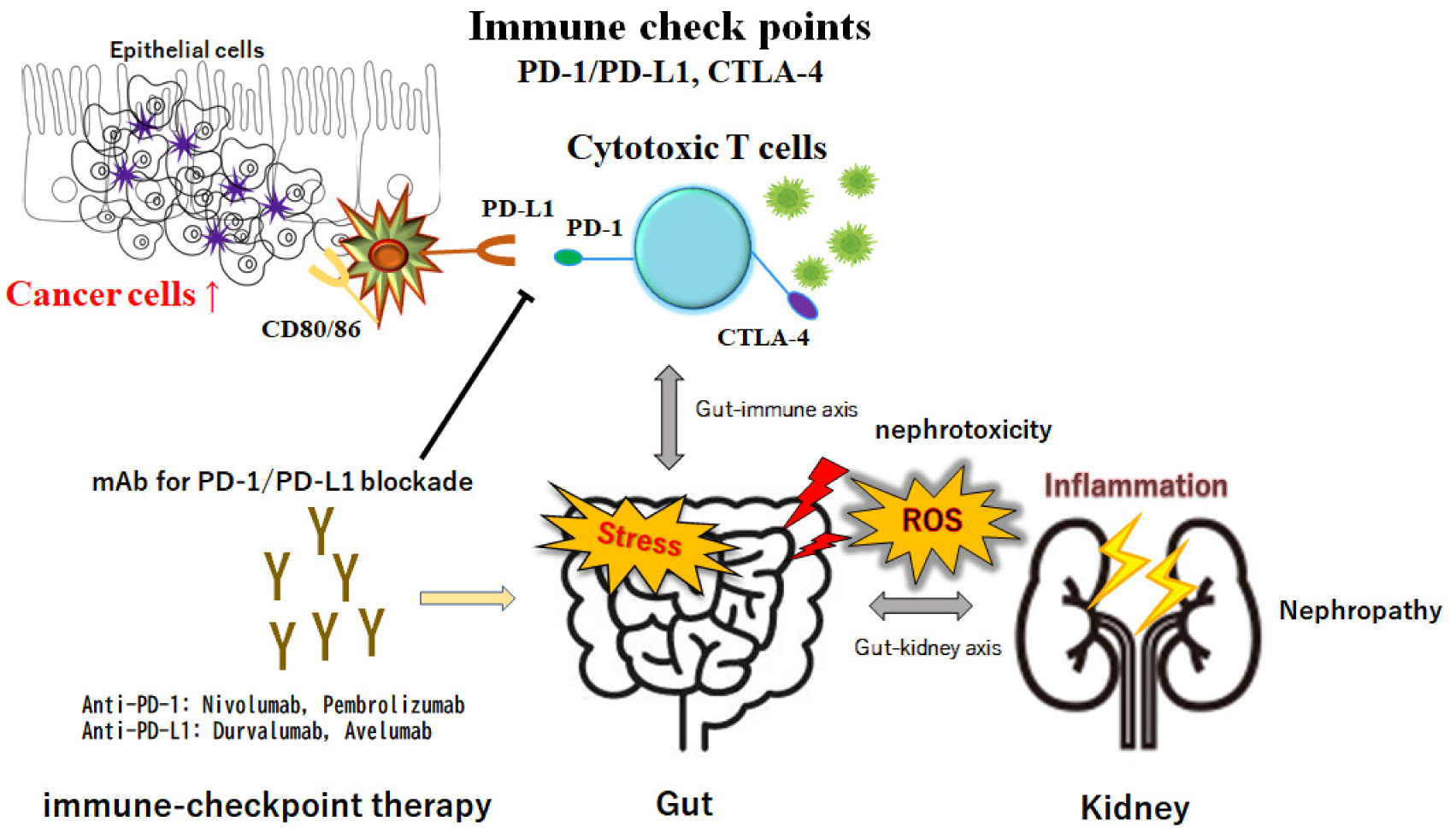
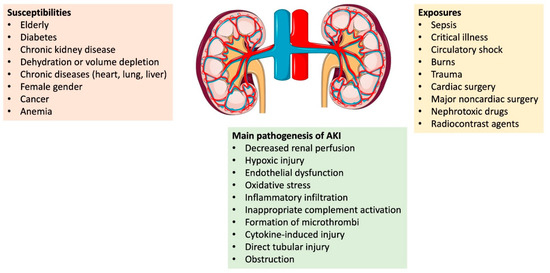
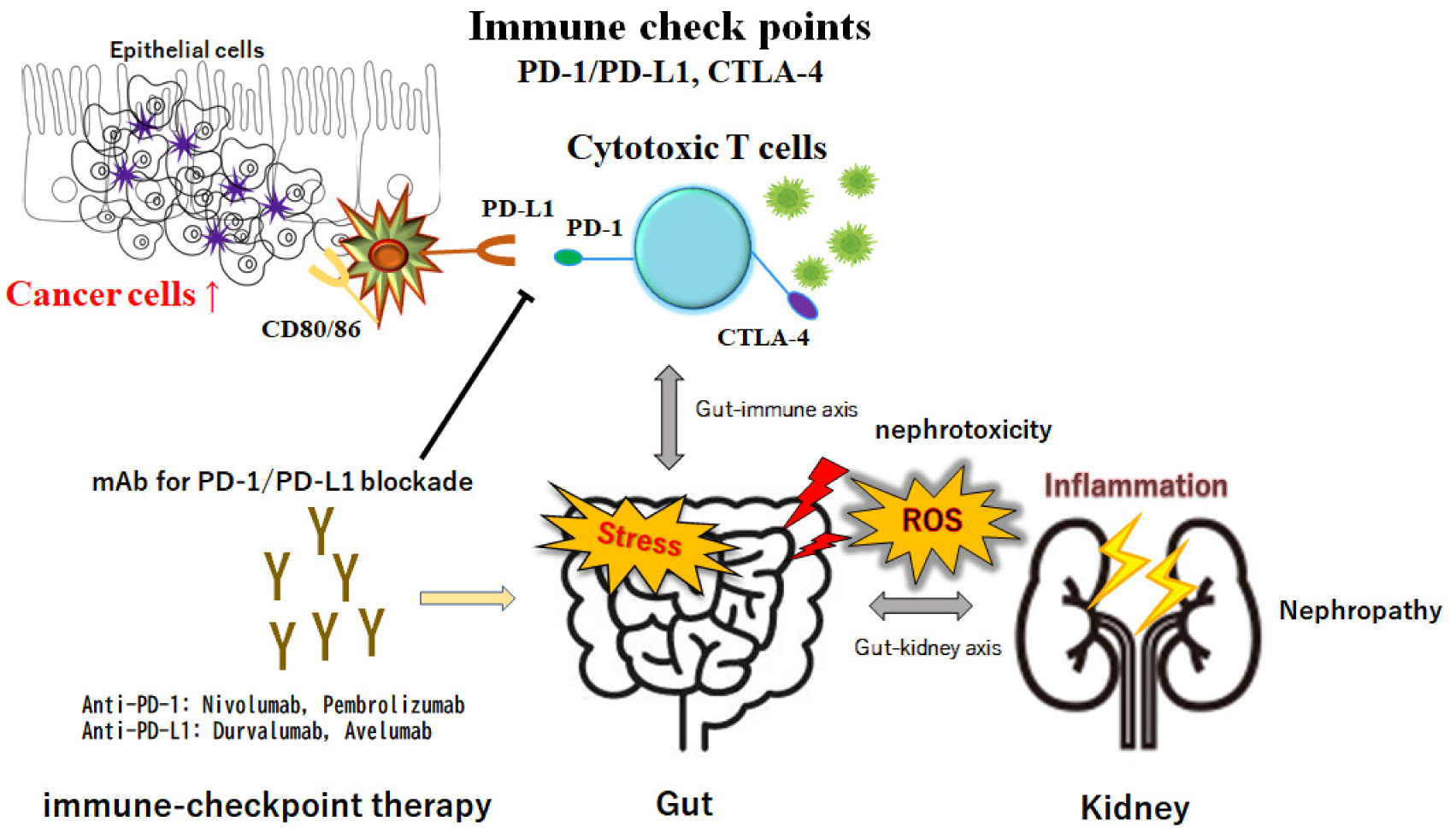
Pharmacology Gabapentin and pregabalin are commonly used first-line agents for diabetic peripheral neuropathy and other common neuropathies. Pharmacologically, both agents inhibit alpha-2-delta (α2δ) subunit of N-type voltage-gated calcium channels, a key receptor involved in regulating the excitability of neurons. 3 Peripheral nerve injury results in the upregulation of α2δ-1 receptors in Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. 1. Introduction Acute kidney injury (AKI) is the sudden loss of kidney function over a period of hours or days. Since the kidneys are one of the major excretory pathways for the removal of drugs from the body, this sudden loss of kidney function can have major implications for a patient’s prescribed medication regime. The term ‘nephrotoxic’ should be used with caution. Few medications Gabapentin toxicity should be considered one of the differential diagnoses of altered consciousness in patients with compromised renal function even after a single dose. We report a 57-year-old woman with diabetes mellitus and uraemia on regular haemodialysis who developed severe dizziness and lethargy after a single recommended dose of gabapentin for bilateral leg dysthesia. Because of Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Existing literature on such risk is lacking. Abstract Background: Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Existing literature on such risk is lacking. Numerous drugs used to manage and treat multiple diseases, including hypertension, diabetes, and other pathologies, are nephrotoxic. These agents are in various classes and categories of medication. This activity reviews the indications, action, and contraindications for nephrotoxic drugs as a valuable agent in choosing key treatment strategies. This activity will highlight the mechanism of Kidney Dysfunction Overview Analgesic prescribing for patients with kidney disease must consider that: (1) some analgesic medications, so called nephrotoxic drugs, can cause kidney injury or worsen kidney function; (2) kidney dysfunction may impair drug elimination, causing or augmenting adverse effects. Discussion: Gabapentin is widely used in the management of pain. It is entirely excreted through the renal system so this needs to be considered in any patient becoming acutely ill and developing renal failure. We describe a patient who developed significant deterioration in her conscious level due to iatrogenic gabapentin overdose. Gabapentin is widely used in the management of pain. It is entirely excreted through the renal system so this needs to be considered in any patient becoming acutely ill and developing renal failure. Gabapentin Effects on Kidneys | Is Gabapentin Bad for Your Kidneys? In this video we talk about Gabapentin effects on kidneys. The question we’re getting a lot is, Is gabapentin bad for kidney disease? Now, gabapentin is a medication used for diabetic neuropathy or neuropathy or any type of nerve pain. Clinical manifestations include increased creatinine levels, swelling, and decreased urine output. Close monitoring of renal function, dosage adjustment based on kidney function, and avoidance of nephrotoxic medications are crucial in managing and preventing gabapentin-related kidney problems. Gabapentin toxicity should be considered one of the differential diagnoses of altered consciousness in patients with compromised renal function, even after a single dose. We report a 57-year-old woman with diabetes mellitus and uraemia on regular Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally Chronic kidney disease affects renal drug elimination and other pharmacokinetic processes involved in drug disposition (e.g., absorption, drug distribution, nonrenal clearance [metabolism]). Drug Gabapentinoids, including gabapentin and pregabalin, are frequently prescribed as opioid alternatives. Given that gabapentinoids are eliminated from the body by the kidney, we sought to determine the risk of serious adverse events in patients with chronic kidney disease who started a gabapentinoid at a higher versus a lower dose. We conducted a population-based study to answer this question As in the other 2 cases of gabapentin-induced acute renal failure and rhabdomyolysis, the patients involved had multiple illnesses and were affected by multiple medications or other factors that might lead to rhabdomyolysis and renal failure. There have also been rare reports linking gabapentin use to acute renal failure or worsening renal function in susceptible individuals. These cases often involve patients who already had underlying renal conditions or who were taking other nephrotoxic medications concurrently. Gabapentin is an anticonvulsant with analgesic effects. It was approved by the Food and Drug Administration in 1994 as an adjunctive agent for partial seizures and subsequently in 2002 as an analgesic for postherpetic neuralgia. In recent years, gabapentin has been increasingly used off-label for expanded indications, including migraine headache,1 phan-tom limb pain,2 cancer-related pain,3 Gabapentin can be used by kidney disease patients, but dosage adjustments are critical. Learn how to safely use gabapentin with kidney issues and discover alternative medications.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |