Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
%20for%20Post-operative%20Pain.png?md=1) |  |
 |  |
 |  |
 |  |
 |  |
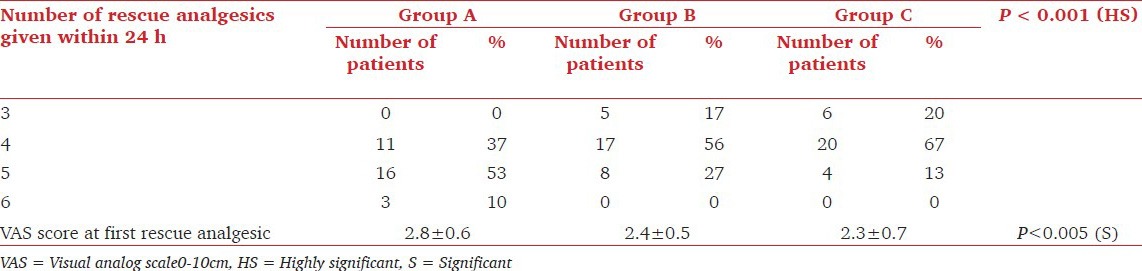
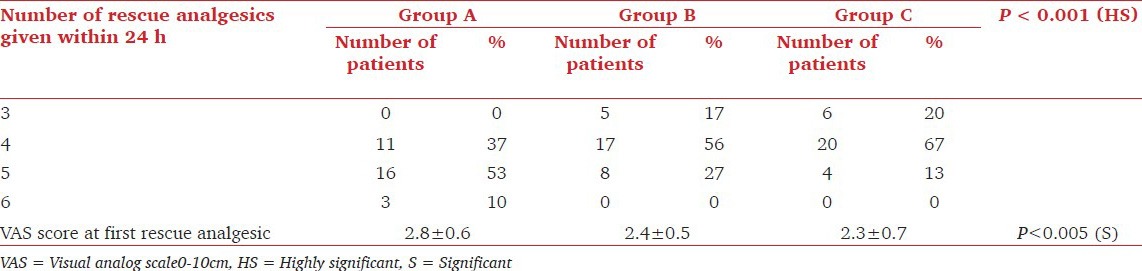
Gabapentin / adverse effects* Gabapentin / analogs & derivatives Humans Meta-Analysis as Topic Pain Management / adverse effects* Pain Management / methods Pain Measurement Pain, Postoperative / diagnosis Pain, Postoperative / drug therapy* Pain, Postoperative / etiology Severity of Illness Index Surgical Procedures, Operative / adverse effects High dose gabapentin taper may be considered for patients with concomitant post-operative pain and alcohol withdrawal to decrease benzodiazepine use (see Alcohol Withdrawal Guideline) Patients on gabapentin prior to admission should be resumed on gabapentin, if clinically appropriate Gabapentin, an anticonvulsant, has recently been suggested as an effective postoperative ‘analgesic’ agent. The objective of the present study was to examine the analgesic effectiveness, opioid-sparing effects and side effects associated with the Abstract Perioperative pain management is a unique challenge in patients undergoing spine surgery due to the increased incidence of both pre-existing chronic pain conditions and chronic postsurgical pain. Peri-operative planning and counseling in spine surgery should involve an interdisciplinary approach that includes consideration of patient-level risk factors, as well as pharmacologic and Firm evidence for use of gabapentin is lacking as clinically relevant beneficial effect of gabapentin may be absent and harm is imminent, especially when added to multi-modal analgesia. Editorial Comment In this trustworthy systematic review, use of gabapentin for post-operative pain management was scrutinized. Background Gabapentin is an antiepileptic drug used in a variety of chronic pain conditions. Increasing numbers of randomized trials indicate that gabapentin is effective as a postoperative analgesic. This procedure-specific systematic review aims to analyse the 24-hour postoperative effect of gabapentin on acute pain in adults. Methods Medline, The Cochrane Library and Google Scholar were The use of gabapentin in the management of postoperative pain after total knee arthroplasty A PRISMA-compliant meta-analysis of randomized controlled trials Post-operative gabapentin (600 mg) may be equally effective as a preoperative dose in decreasing PACU narcotic use. Level 3 Concomitant administration of gabapentin as part of a multi-modal pain management strategy including narcotics, non-steroidal anti-inflammatory drugs (NSAIDS), and muscle relaxants does not improve pain scores. Prescription of gabapentin and pregabalin in the perioperative period has become increasingly common, if not de rigueur. These gabapentinoids have become ubiquitous components of protocols for early recovery after surgery and multi-modal analgesia. Neither is approved by the US Food and Drug Administration (FDA) for preventing or treating surgical pain, but their use is predicated on Gabapentin may be prescribed either before or after surgery to help with postsurgical pain. However, it should be used with caution due to the high risk of abuse. Conclusions: Gabapentin appears safe and well tolerated when used for persistent post-operative and post-traumatic pain in thoracic surgery patients, although minor side effects do occur. Gabapentin may relieve refractory chest wall pain in some of these patients, particularly those with more severe pain. This review evaluated the efficacy and tolerability of peri-operative gabapentin administration to control acute post-operative pain. Peri-operative gabapentin administration was found to be effective in reducing pain scores, opioid requirements and opioid-related adverse effects in the first 24 hours after surgery. Given the significant differences between the studies and the possibility of In recent years, there has been increased interest in using gabapentinoids (gabapentin and pregabalin) as part of multimodal medication plans or enhanced recovery after surgery protocols to mitigate several perioperative clinical challenges. Abstract Background: Perioperative pain treatment often consist of combinations of non-opioid and opioid analgesics, 'multimodal analgesia', in which gabapentin is currently used. The aim was to document beneficial and harmful effects of perioperative gabapentin treatment. This randomized clinical trial evaluates the effects of perioperative administration of gabapentin on postoperative pain resolution and time to cessation of opioid use. Gabapentin is a novel drug used for the treatment of postoperative pain with antihyperalgesic properties and a unique mechanism of action, which differentiates it from other commonly used drugs. Various studies have shown that perioperative use of gabapentin reduces postoperative pain. The shift towards multimodal pain regimens, including gabapentin, has taken place without attention to ensuring that they, like opioids, are appropriately discontinued soon after surgery. The prevalence of prolonged use of post-operative gabapentin among older adults is unknown, as are the factors associated with prolonged use. These results were consistent regardless of the type of drug (gabapentin or pregabalin). No effect was observed on pain intensity at 72 h, subacute and chronic pain. The use of gabapentinoids was associated with a lower risk of postoperative nausea and vomiting but with more dizziness and visual disturbance. In 2002, its indications were expanded to include the management of post-herpetic neuralgia, which is neuropathic pain that occurs following shingles, as well as other painful neuropathies and nerve-related pain [14]. Gabapentin is classified as an anticonvulsant and has demonstrated efficacy in managing neuropathic and chronic pain [15, 16]. Gabapentin, an anticonvulsant, recently has been suggested as an effective post-operative “analgesic” agent. The objective of the present study was to examine the analgesic effectiveness and opioid-sparing effects associated with the use of a single
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
%20for%20Post-operative%20Pain.png?md=1) |  |
 |  |
 |  |
 |  |
 |  |