Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 | 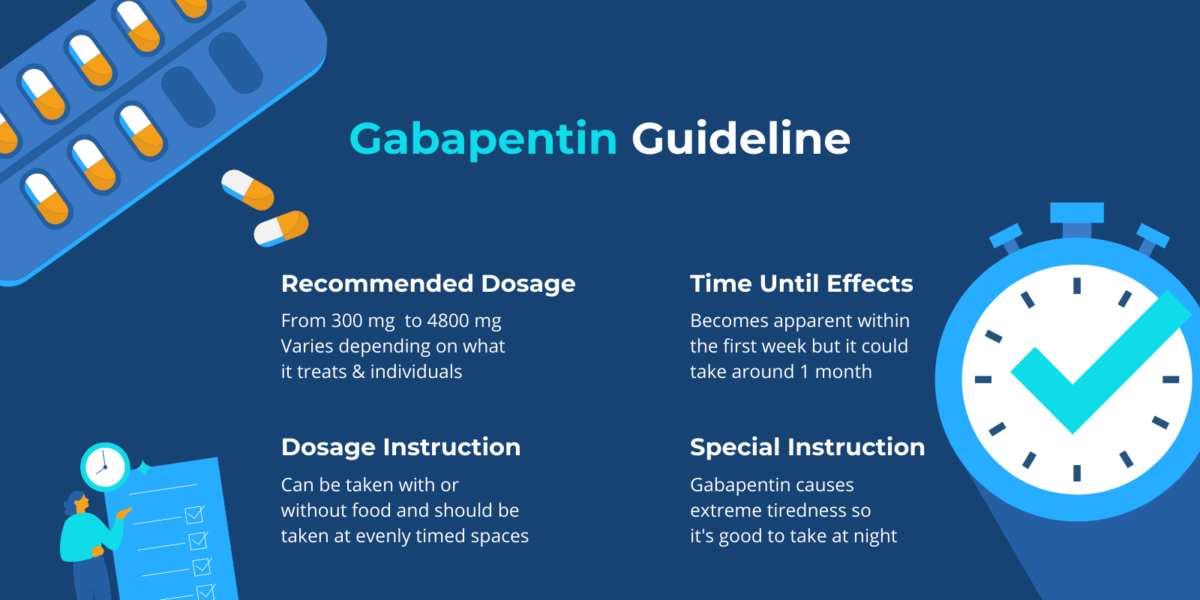 |
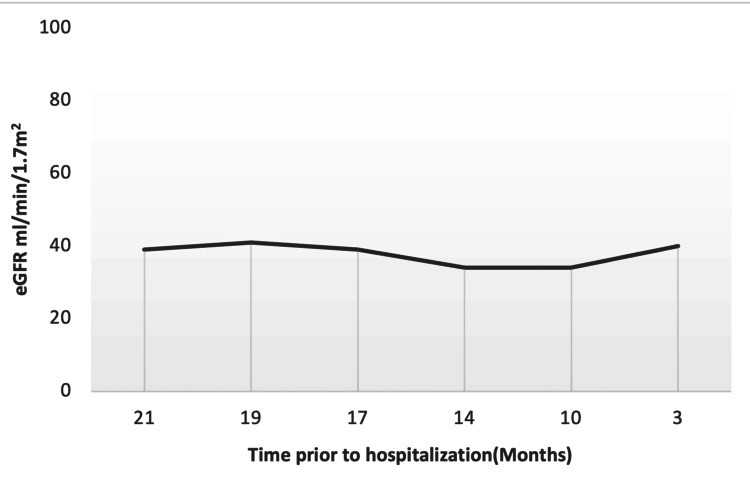
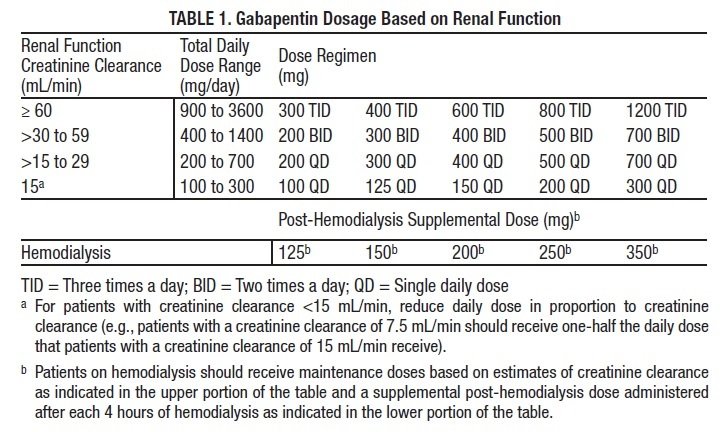
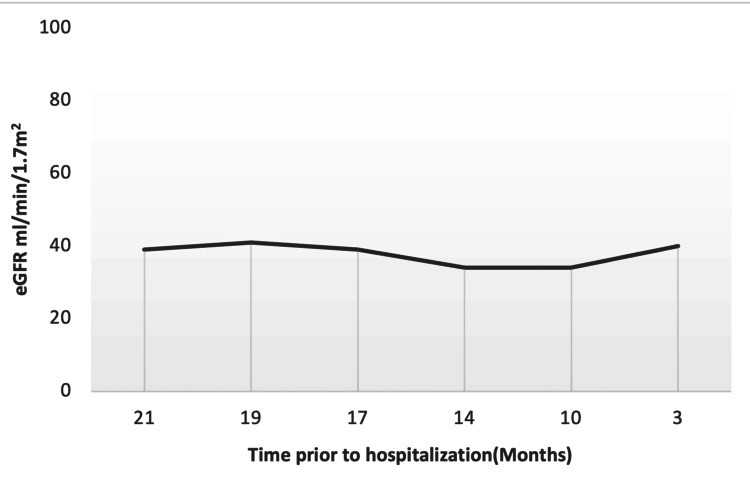
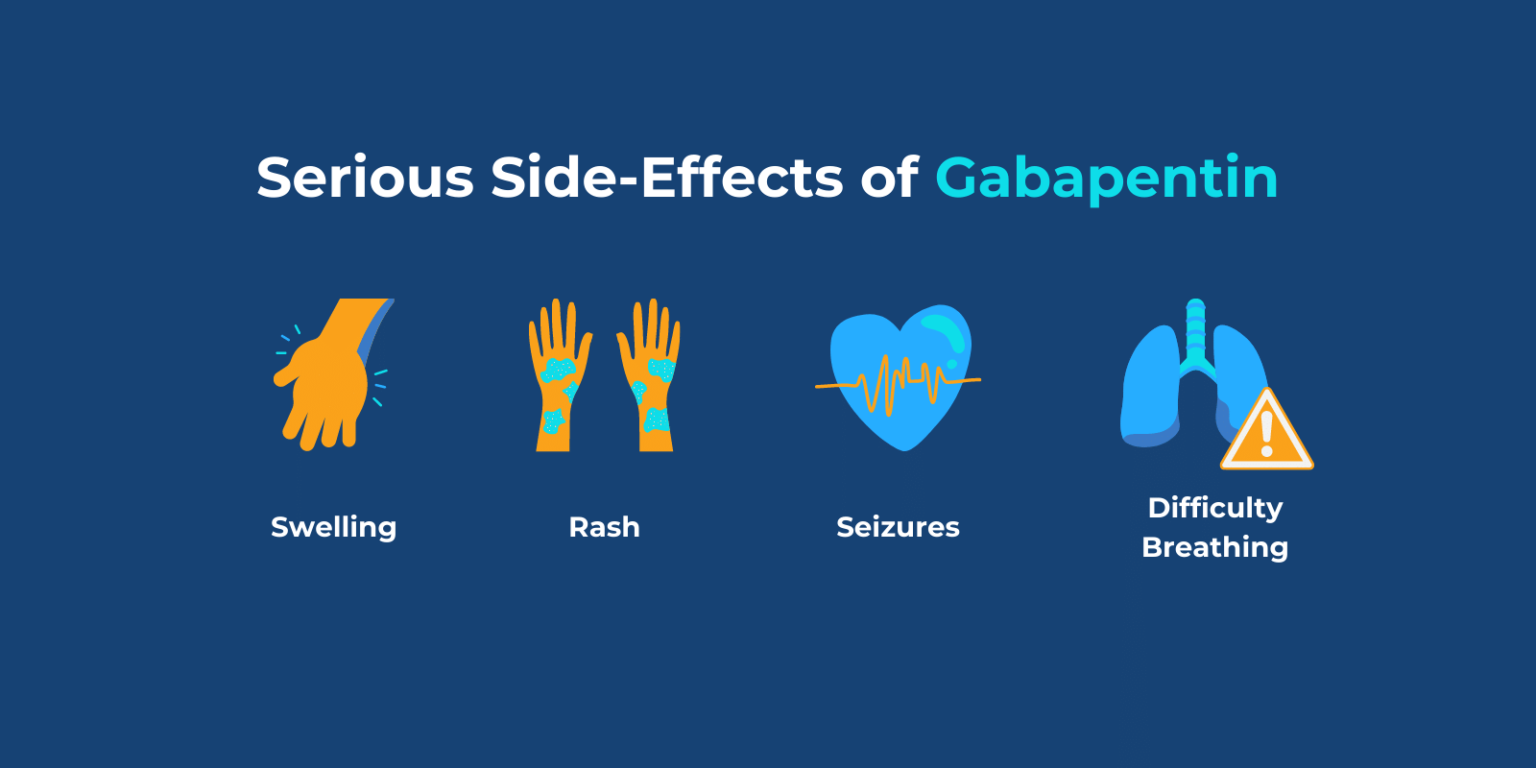
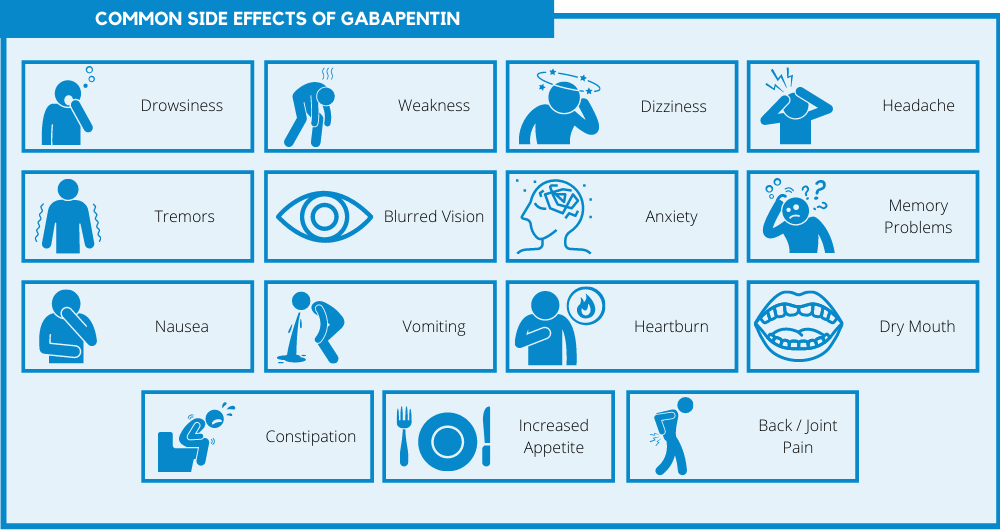
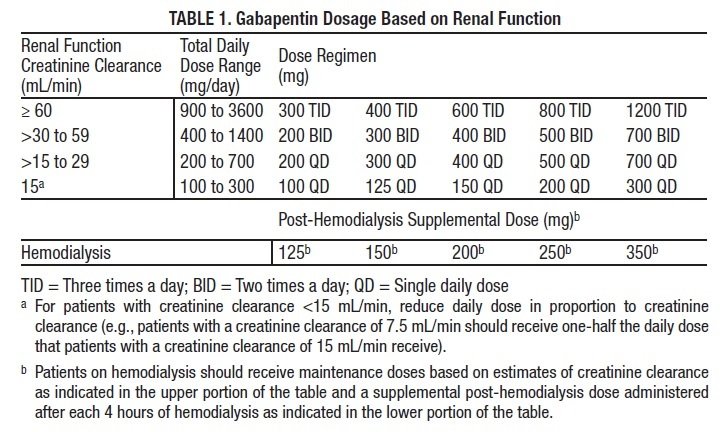
Abstract Background: Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Existing literature on such risk is lacking. Patients with chronic kidney disease often receive inappropriately high gabapentin dosage for their kidney function, occasioning overt toxicity; advanced age and comorbidity predispose these patients for toxicity. Studies have shown that gabapentin toxicity can occur in patients with chronic kidney disease, particularly in those with advanced age and multiple comorbidities 4, 5. Dose Adjustment and Renal Function Dose adjustment of gabapentin is crucial in patients with decreased renal function to prevent toxicity 4, 5. Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Existing literature on such risk is lacking. The appropriate dosing based on the patient’s actual creatinine clearance is imperative to prevent severe adverse side effects and drug-related toxicity. We report a case of myoclonic activity developed in a patient with chronic kidney disease (CKD) shortly after a gabapentin dose increase. Case presentation Discussion: Gabapentin is widely used in the management of pain. It is entirely excreted through the renal system so this needs to be considered in any patient becoming acutely ill and developing renal failure. We describe a patient who developed significant deterioration in her conscious level due to iatrogenic gabapentin overdose. Abstract Gabapentin is frequently used as an analgesic in patients with chronic kidney disease (CKD). It is excreted exclusively through kidney, and therefore impairment in kidney function could lead to gabapentin accumulation and hence toxicity. We present our experience of 3 cases with Gabapentin toxicity who were managed according to the severity of symptoms. Case 1: A 32-year-old male was Gabapentinoids, including gabapentin and pregabalin, are frequently prescribed as opioid alternatives. Given that gabapentinoids are eliminated from the body by the kidney, we sought to determine the risk of serious adverse events in patients with chronic kidney disease who started a gabapentinoid at a higher versus a lower dose. Discussion. Gabapentin is widely used in the management of pain. It is entirely excreted through the renal system so this needs to be considered in any patient becoming acutely ill and developing renal failure. We describe a patient who developed significant deterioration in her conscious level due to iatrogenic gabapentin overdose. Conclusion. Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Existing literature on such risk is lacking. About safe medication use with chronic kidney disease Medications are a very important part of staying healthy, especially if you have chronic kidney disease (CKD). But all medicines bring some level of risk for side effects and other safety concerns. Some medicines can damage your kidneys. Abstract Background: Gabapentinoids (GPs) are frequently prescribed in individuals with chronic kidney disease (CKD); however, their exclusive renal elimination warrants dose adjustments to decrease risk of toxicity. This study evaluated GP prescribing patterns and whether excessive dosing was associated with increased incidence of gabapentinoid-related adverse events (GRAEs). Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Existing literature on such risk is lacking. Rowland–Tozer method. Conclusion Gabapentin and pregabalin are commonly used for neuropathic pain in CKD patients but are not fully understood as this population remains excluded from efficacy and safety trials. Renal adjustments for the gabapentinoids are prodigiously recommended in the literature. However, current guidance is based on pharmacokinetic and toxicity studies, but studies Gabapentin can be used by kidney disease patients, but dosage adjustments are critical. Learn how to safely use gabapentin with kidney issues and discover alternative medications. Gabapentin is frequently used as an analgesic in patients with chronic kidney disease (CKD). It is excreted exclusively through kidney, and therefore impairment in kidney function could lead to Gabapentin toxicity and side effects are well-known among nephrologists and fully described in the literature as myoclonic twitches, myopathy, neurotoxicity, etc., particularly in dialysis patients. 2,4 Rhabdomyolysis with associated acute renal failure is an uncommon side effect, but it has been described in earlier cases. 1,3 Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Existing literature on such risk is lacking. Since gabapentin is cleared solely by renal excretion, dosing requires consideration of the patient's renal function. Myoclonic activity may occur as a complication of gabapentin toxicity, especially with acute kidney injury or end-stage renal disease. Gabapentin is actually toxic to the kidneys. Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its well recieved pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |