Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 | |
 |  |
 |  |
 |  |
 |  |
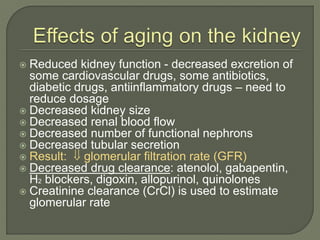
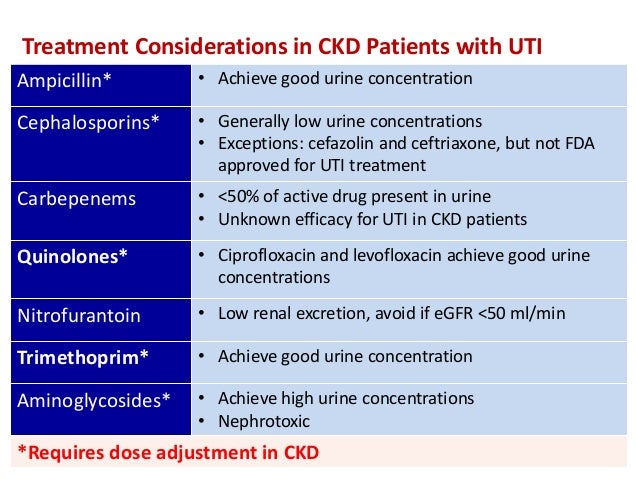
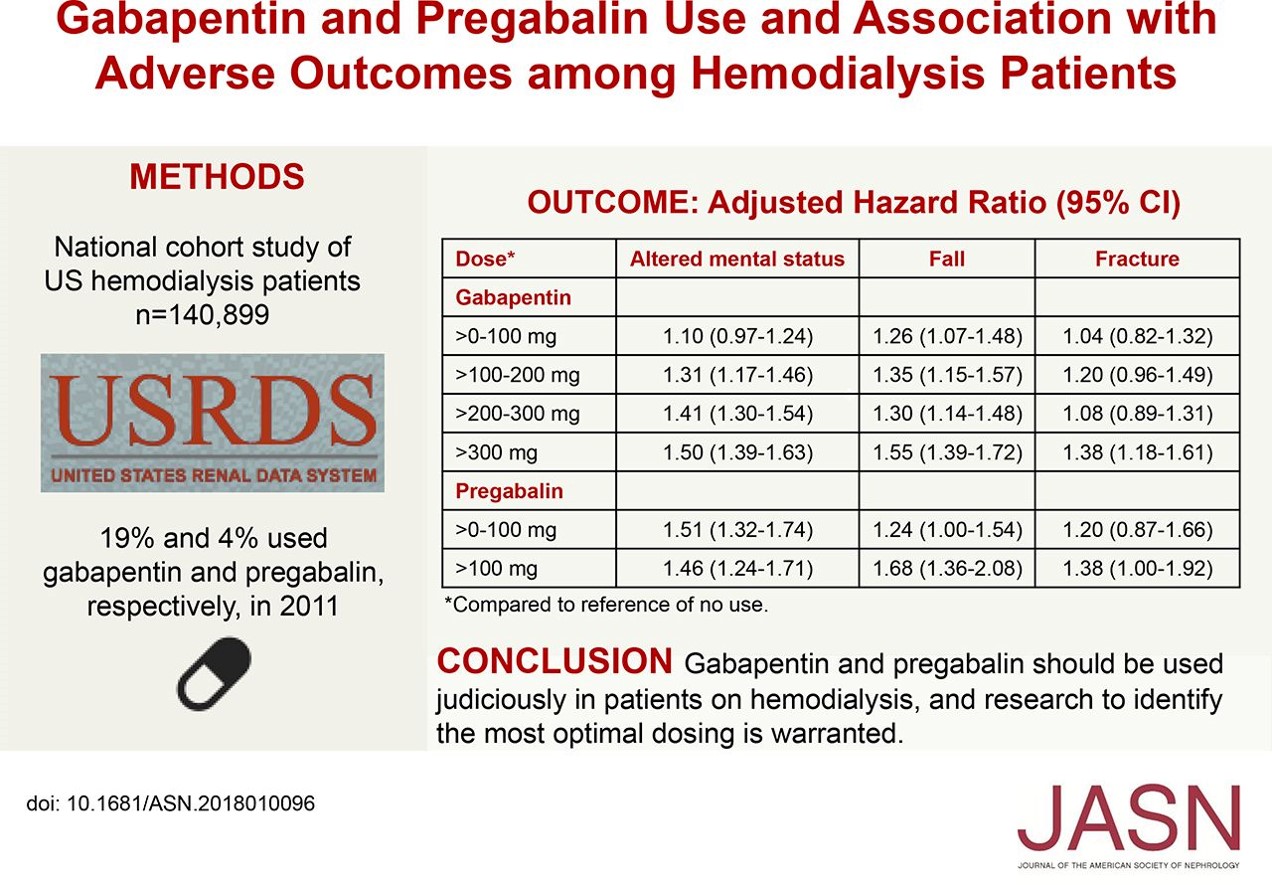
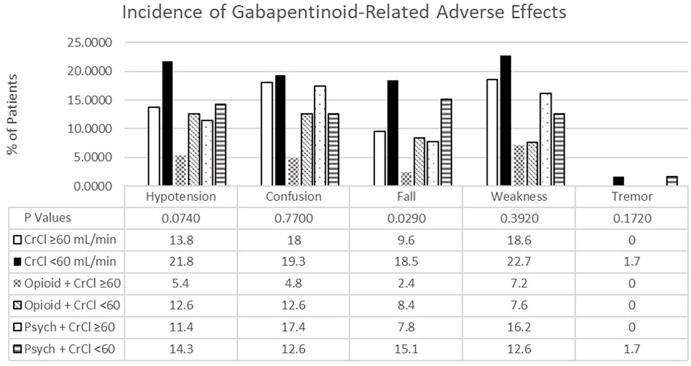
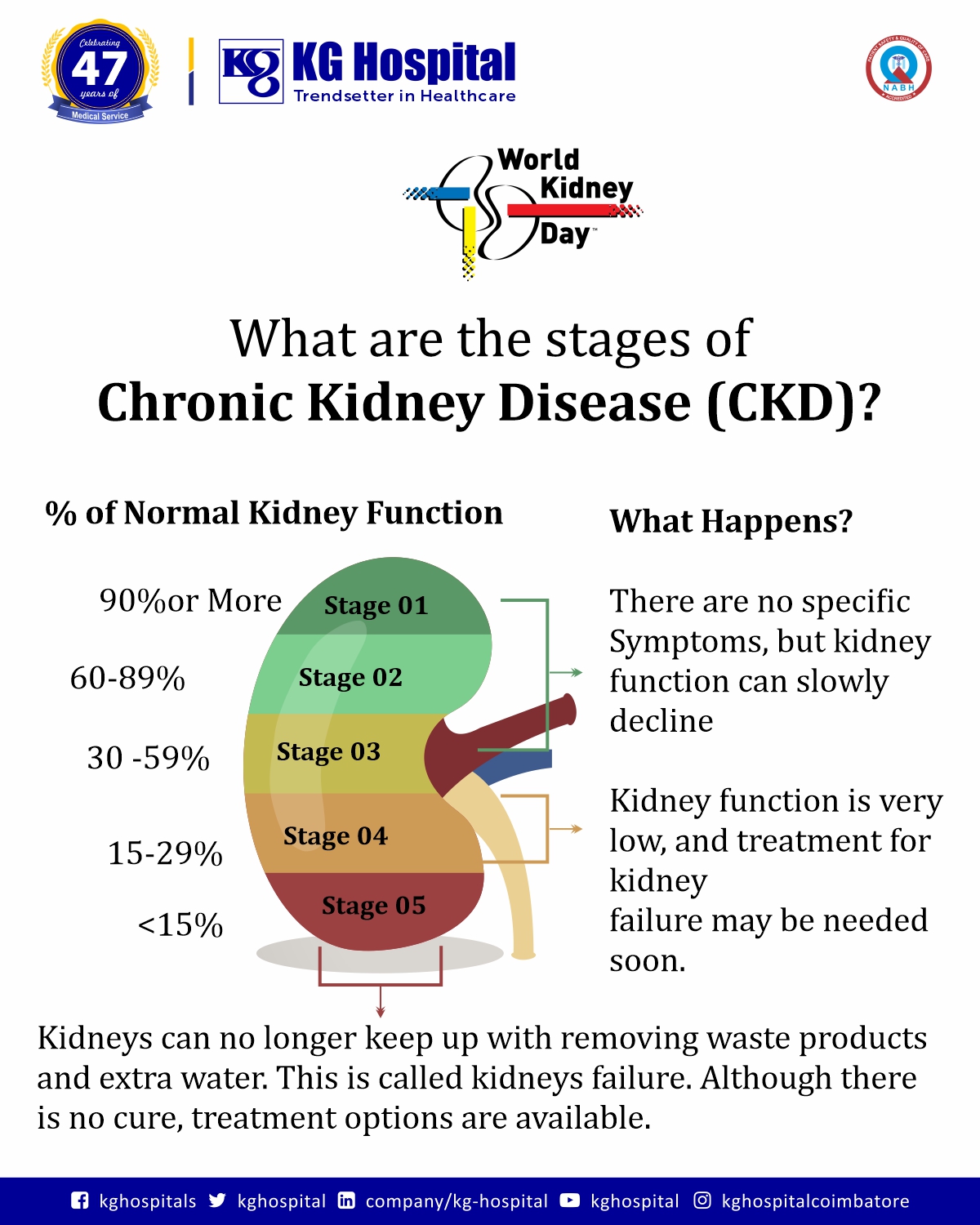
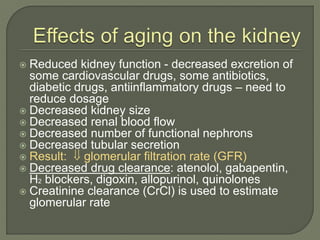
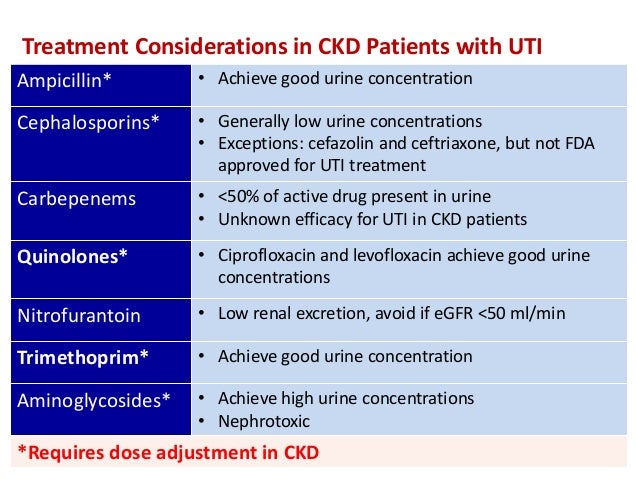
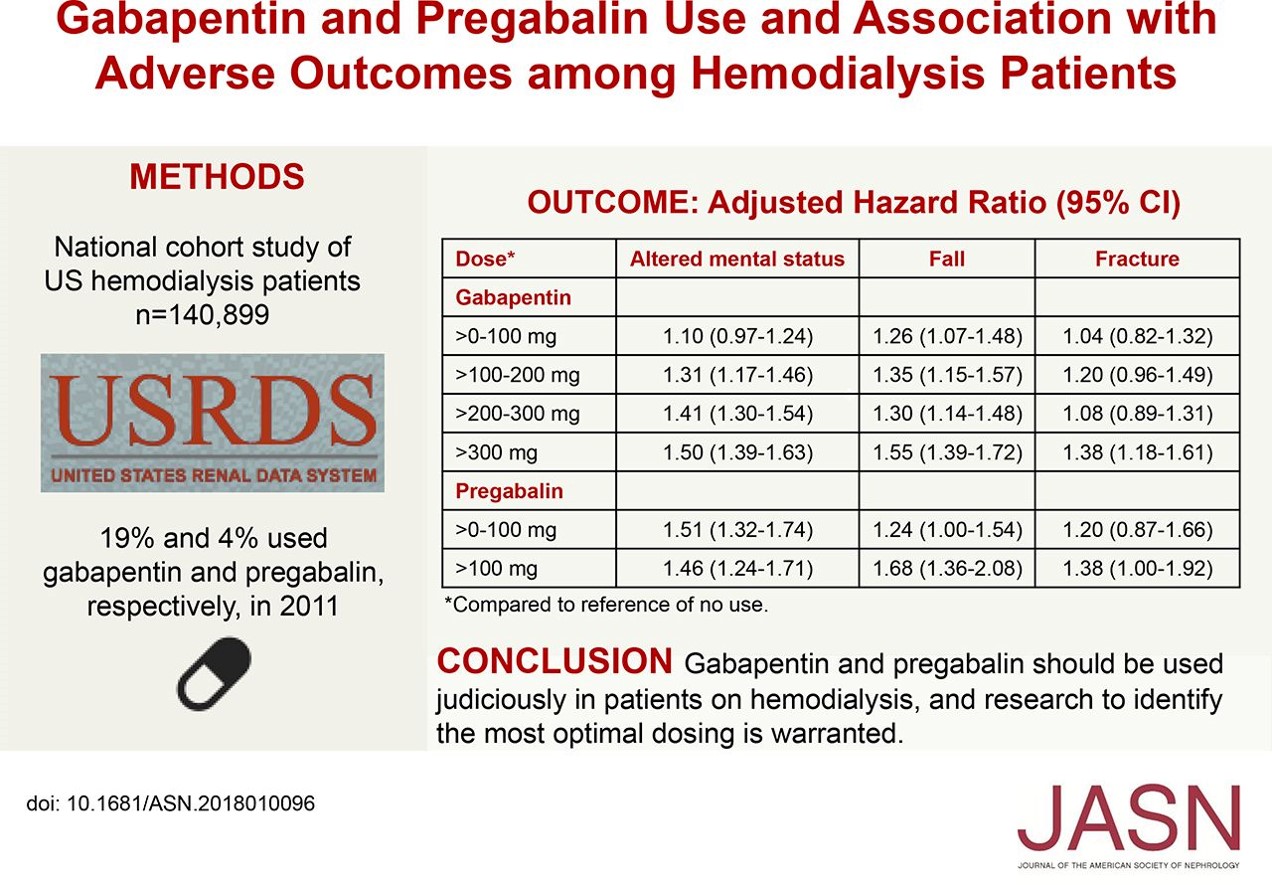
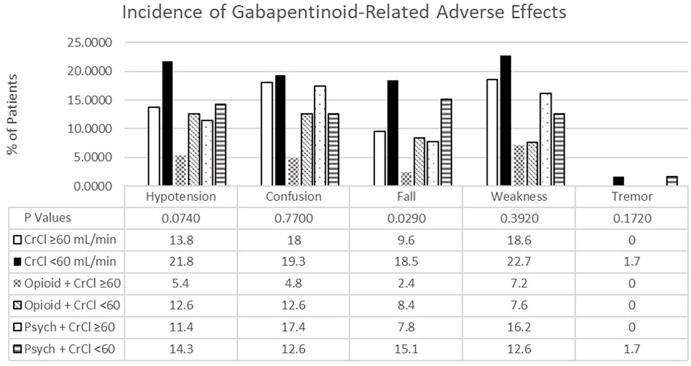
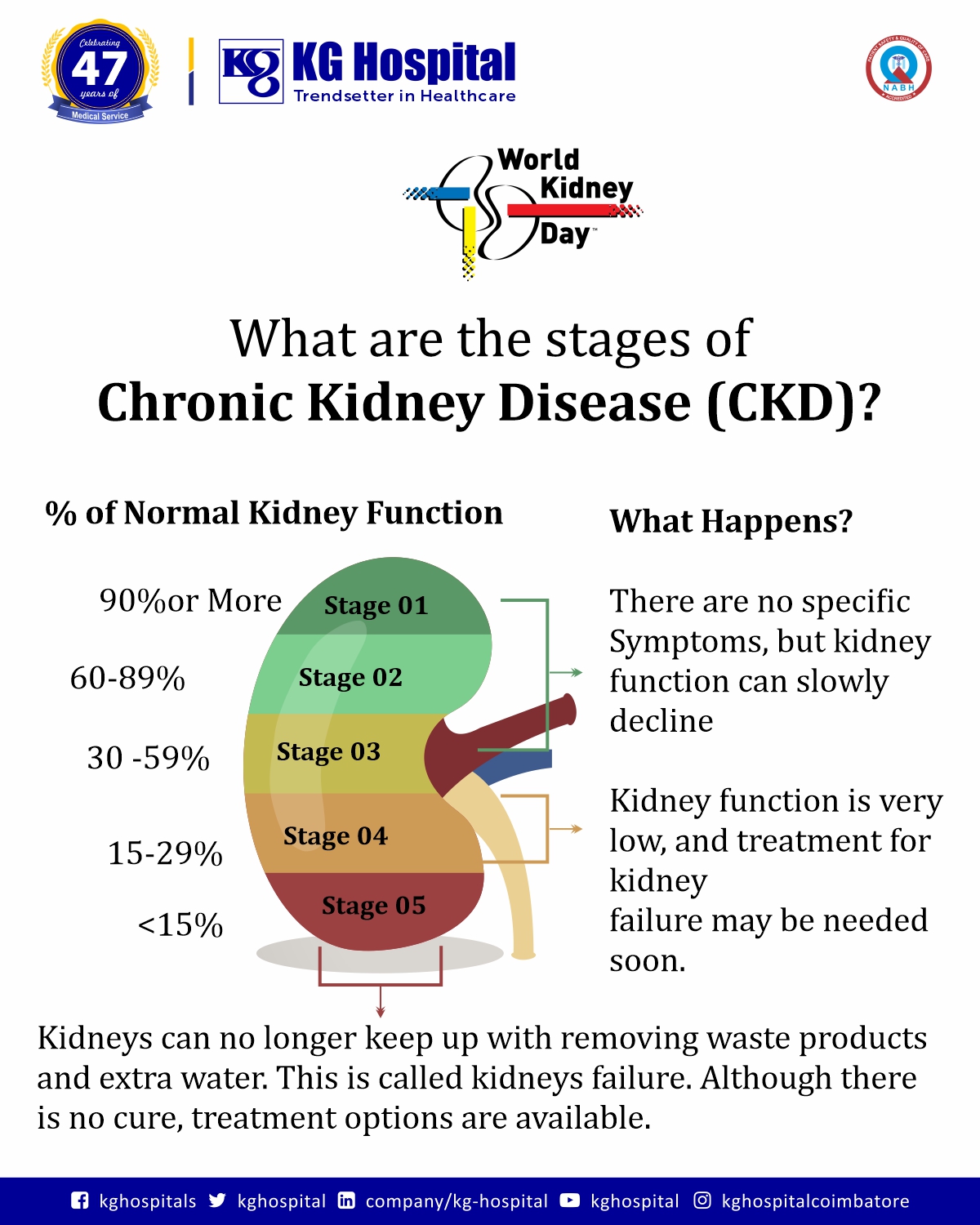
Abstract Background: Gabapentin and pregabalin are well-tolerated medications primarily cleared by the kidney. Patients receiving higher gabapentinoid doses with decreased kidney function may be at an increased risk of adverse effects (AEs), but limited evidence exists evaluating gabapentinoid dosing and AEs in this population. Gabapentin is actually toxic to the kidneys. Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its well recieved pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Physicians should be familiar with commonly used medications that require dosage adjustments. Resources are available to assist in dosing decisions for patients with chronic kidney disease. Gabapentin impacts kidney function by reducing its ability to clear the drug, leading to its accumulation and potential damage. Clinical manifestations include increased creatinine levels, swelling, and decreased urine output. Gabapentin is widely used in the management of pain. It is entirely excreted through the renal system so this needs to be considered in any patient becoming acutely ill and developing renal failure. Key Takeaways: Can Gabapentin Cause Kidney Problems? Gabapentin is primarily processed by the kidneys. Kidney function should be monitored during treatment. Dosage adjustments may be necessary for renal impairment. Some patients report mild kidney-related side effects. Consult a doctor if experiencing unusual symptoms. Here’s a scenario of using gabapentin in chronic kidney disease. A 42 year old African American man with a history of coronary artery disease and decompensated heart failure s/p heart transplant and chronic kidney disease presented to a hospital on 9/29/16 complaining of shortness of breath, dyspnea upon exertion and LE edema. Gabapentin’s apparent total clearance is 100 mL/min in adults with normal renal function, which is essentially equivalent to CrCl and does not suggest the involvement of tubular reabsorption. 1 Some evidence suggest that active tubular secretion mediated by organic cation transporter-1 (OCT-1) may play a role in gabapentin’s renal clearance. The dependence on the kidney for gabapentin excretion can lead to toxicity in people with decreased kidney function.6,7 Manifestations of toxicity include dizziness, confusion, lethargy, myoclonus, ataxia, and tremulousness.6 The therapeutic range for gabapentin in blood is about 2 to 20 mg/mL (12-120 mol/L), m Gabapentinoids are opioid substitutes whose elimination by the kidneys is reduced as kidney function declines. To inform their safe prescribing in older adults with chronic kidney disease (CKD), we examined the 30-day risk of serious adverse events according to the prescribed starting dose. Conclusion Gabapentin toxicity in patients with chronic kidney disease is underrecognized. Patients with chronic kidney disease often receive inappropriately high gabapentin dosage for their kidney function, occasioning overt toxicity; advanced age and comorbidity predispose these patients for toxicity. For people with normal kidney function, gabapentin is safe and doesn’t cause kidney complications or trigger kidney disease. In people with renal impairment, gabapentin can be harder to clear from the body. People with kidney disease may be prescribed gabapentin, but their dose will need to be lowered based on how well their kidneys function. Abstract Background: Gabapentin and pregabalin are well-tolerated medications primarily cleared by the kidney. Patients receiving higher gabapentinoid doses with decreased kidney function may be at an increased risk of adverse effects (AEs), but limited evidence exists evaluating gabapentinoid dosing and AEs in this population. Objective: To determine whether patients with decreased creatinine The exact renal dosing for gabapentin is not specified in the provided studies, but it is recommended to use gabapentin judiciously in patients with decreased kidney function and to consider dosage adjustments based on the patient's creatinine clearance (CrCl) 4, 5. Gabapentinoids are opioid substitutes whose elimination by the kidneys is reduced as kidney function declines. To inform their safe prescribing in older adults with chronic kidney disease (CKD), we examined the 30-day risk of serious adverse events according to the prescribed starting dose. This is a severe allergic reaction that can cause damage to major organs, including the liver and kidneys. If you have existing kidney problems, you may need a lower dose of gabapentin. This is because the kidneys help the body get rid of gabapentin. If you have impaired kidney function, gabapentin may build up in the body and cause side effects. Abstract Background: Gabapentin and pregabalin are well-tolerated medications primarily cleared by the kidney. Patients receiving higher gabapentinoid doses with decreased kidney function may be at an increased risk of adverse effects (AEs), but limited evidence exists evaluating gabapentinoid dosing and AEs in this population. Neurontin - Gabapentin Renal Dosing protocol for Adults, maintenance gabapentin dosing and additional dosing for adults undergoing dialysis Studies have shown that gabapentin toxicity can occur in patients with chronic kidney disease, particularly in those with advanced age and multiple comorbidities 4, 5. Dose Adjustment and Renal Function Dose adjustment of gabapentin is crucial in patients with decreased renal function to prevent toxicity 4, 5. Conclusion: Gabapentin toxicity in patients with chronic kidney disease is underrecognized. Patients with chronic kidney disease often receive inappropriately high gabapentin dosage for their kidney function, occasioning overt toxicity; advanced age and comorbidity predispose these patients for toxicity. Heightened awareness of such preventable risk, amid the chronic kidney disease epidemic
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 | |
 |  |
 |  |
 |  |
 |  |