Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
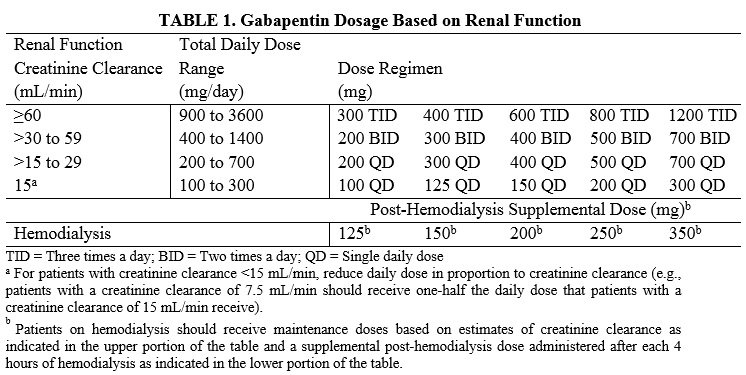
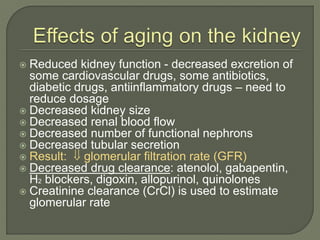
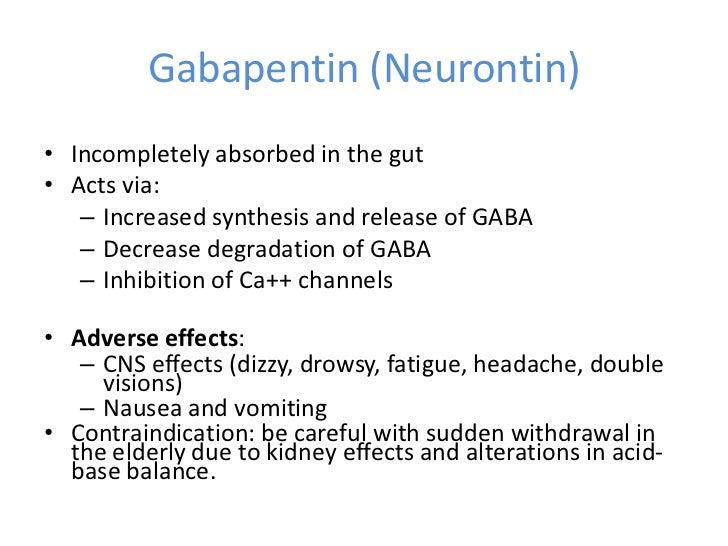
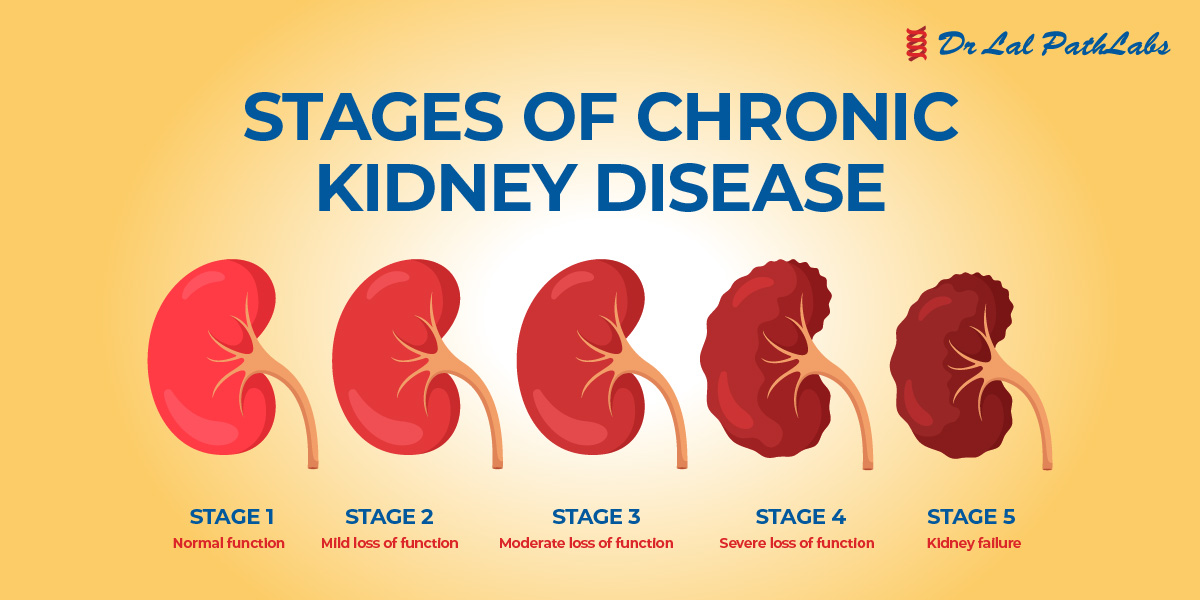
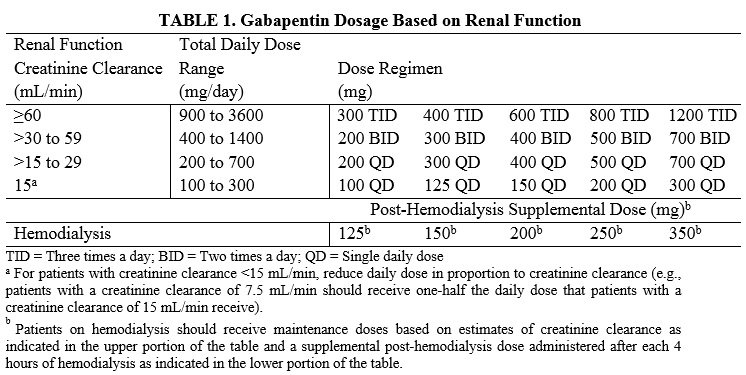
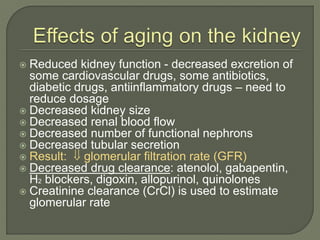
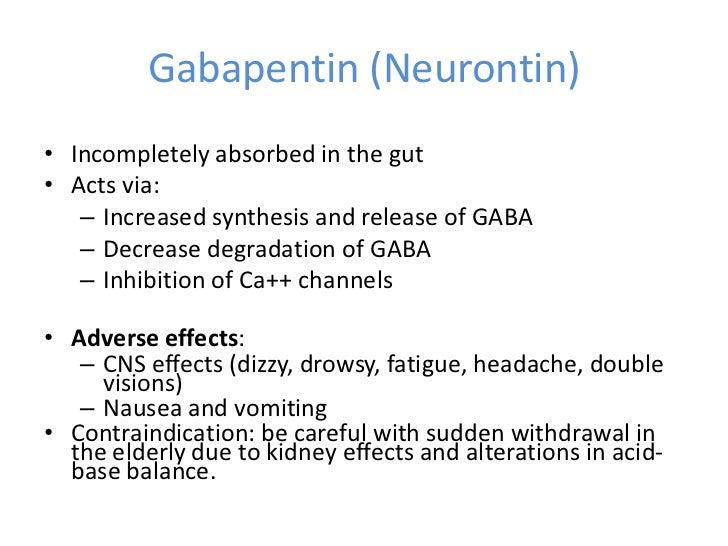
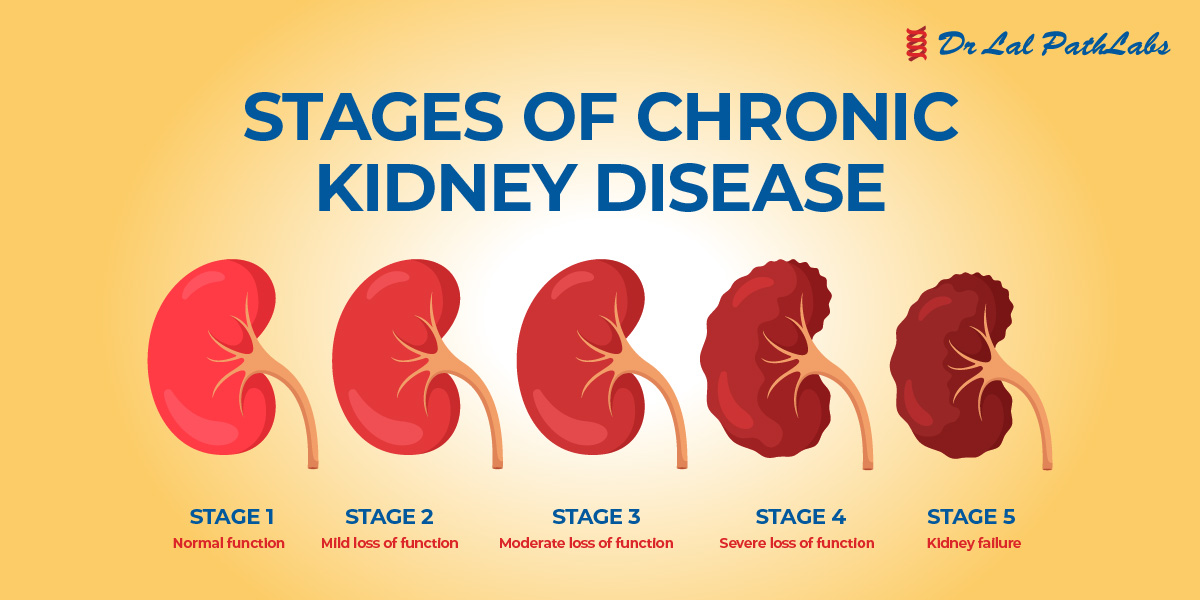
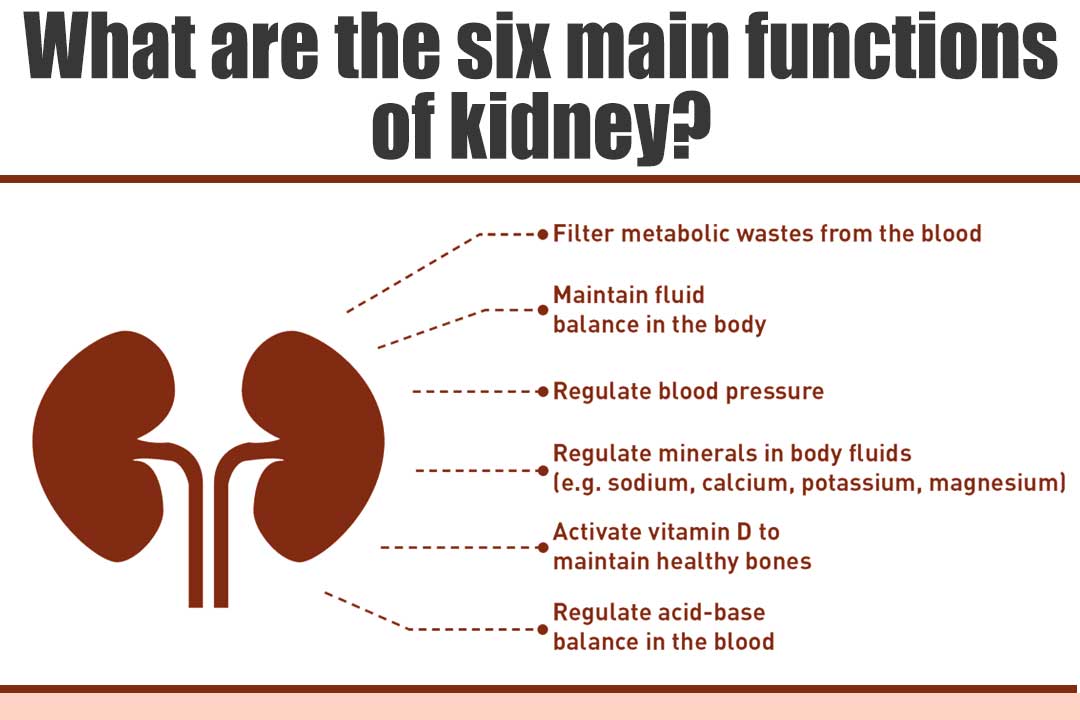
Gabapentin, a medication primarily used to treat nerve pain and seizures, has garnered attention for its efficacy and safety profile. However, concerns about its potential impact on kidney health have emerged, especially among patients with pre-existing kidney conditions. Understanding the relationship between gabapentin and kidney function is crucial for both patients and healthcare providers. Gabapentinoids, including gabapentin and pregabalin, are frequently prescribed as opioid alternatives. Given that gabapentinoids are eliminated from the body by the kidney, we sought to determine the risk of serious adverse events in patients with chronic kidney disease who started a gabapentinoid at a higher versus a lower dose. Here’s a scenario of using gabapentin in chronic kidney disease. A 42 year old African American man with a history of coronary artery disease and decompensated heart failure s/p heart transplant and chronic kidney disease presented to a hospital on 9/29/16 complaining of shortness of breath, dyspnea upon exertion and LE edema. Gabapentin can be used by kidney disease patients, but dosage adjustments are critical. Learn how to safely use gabapentin with kidney issues and discover alternative medications. When kidney function declines, the clearance of Gabapentin can be affected, leading to increased levels in the bloodstream. For patients with normal kidney function, Gabapentin's half-life—approximately 5 to 7 hours—allows for effective dosing without significant accumulation. Managing pain in dogs with kidney disease can be challenging, as many medications can worsen kidney function. Finding safe and effective pain relief requires a thoughtful, well-balanced approach to avoid aggravating your dog’s kidney condition while still alleviating discomfort. Key Takeaways: Quick Answers for Dogs with Kidney Disease What’s the safest pain medication? 🩺 Gabapentin and Abstract Background: Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Existing literature on such risk is lacking. Background: Gabapentin and pregabalin are well-tolerated medications primarily cleared by the kidney. Patients receiving higher gabapentinoid doses with decreased kidney function may be at an increased risk of adverse effects (AEs), but limited Gabapentin is widely used in the management of pain. It is entirely excreted through the renal system so this needs to be considered in any patient becoming acutely ill and developing renal failure. Gabapentinoids are eliminated from the body solely by the kidney, and pharmacokinetic studies show a stepwise prolongation in the elimination half-life of gabapentin and pregabalin as kidney function declines. 9,10 Gabapentinoids should therefore be started at lower doses in patients with chronic kidney disease (CKD; guidelines are summarized This is a severe allergic reaction that can cause damage to major organs, including the liver and kidneys. If you have existing kidney problems, you may need a lower dose of gabapentin. This is because the kidneys help the body get rid of gabapentin. If you have impaired kidney function, gabapentin may build up in the body and cause side effects. Gabapentin toxicity in patients with chronic kidney disease is underrecognized. Patients with chronic kidney disease often receive dangerously high gabapentin dosage for their kidney function, which can lead to all sorts of problems. Gabapentin can be removed from plasma by hemodialysis. Gabapentin affects kidney function as it is primarily eliminated by the kidneys and its clearance is directly proportional to creatinine clearance. This means that patients with impaired renal function may have reduced gabapentin clearance, leading to increased drug levels and potential The exposure of interest was the initiation of pregabalin or gabapentin during the perioperative period. The primary outcome was renal function decline. Secondary outcomes included incident chronic kidney disease (CKD), hospital-acquired acute kidney injury (AKI), and in-hospital mortality. The exact renal dosing for gabapentin is not specified in the provided studies, but it is recommended to use gabapentin judiciously in patients with decreased kidney function and to consider dosage adjustments based on the patient's creatinine clearance (CrCl) 4, 5. Learn about eGFR, a key indicator of kidney health. Understand what your eGFR means, how it's calculated, and steps to maintain healthy kidney function. Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. Existing literature on such risk is lacking. Pain medicines A common class of pain medicines known as “non-steroidal anti-inflammatory drugs” or NSAIDs can lower the amount of blood flowing to your kidneys. This can raise your blood pressure and cause kidney damage, especially with high doses and/or long-term use. Gabapentin’s apparent total clearance is 100 mL/min in adults with normal renal function, which is essentially equivalent to CrCl and does not suggest the involvement of tubular reabsorption. 1 Some evidence suggest that active tubular secretion mediated by organic cation transporter-1 (OCT-1) may play a role in gabapentin’s renal clearance. 5. Peadiatric Renal Dosing For Children: Kidney Function: If a child has kidney problems, the dose needs to be lower. Ages ≥12 years: Adjust based on creatinine clearance and weight. Dosage Adjustment: Lower doses required; consult a paediatric specialist. 6. Administration How to Take Gabapentin: Gabapentin Capsules/Extended-Release:
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |