Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
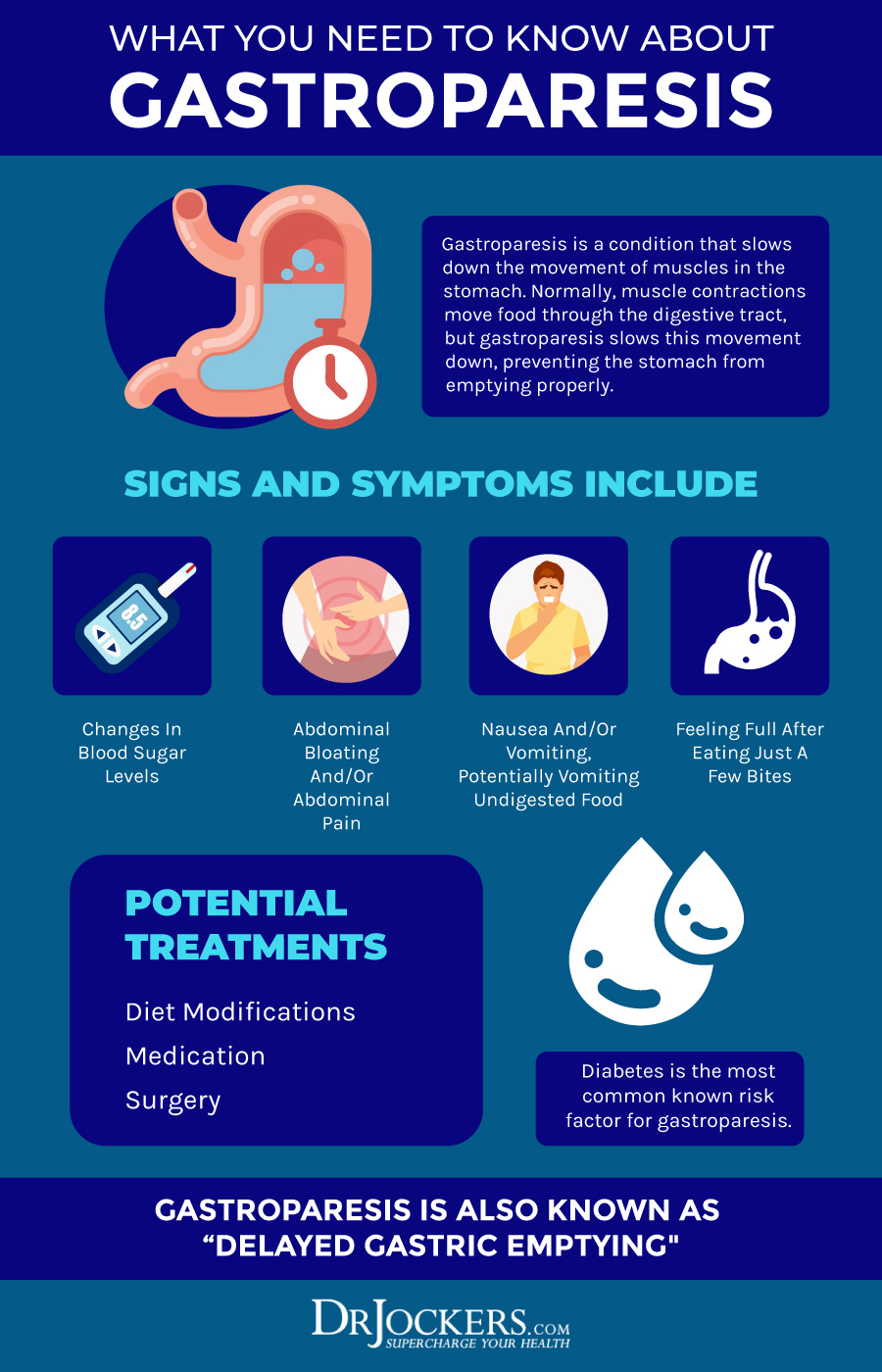 | 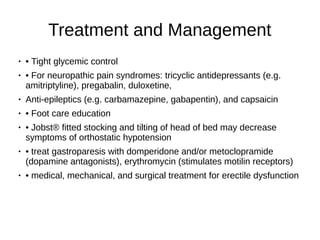 |
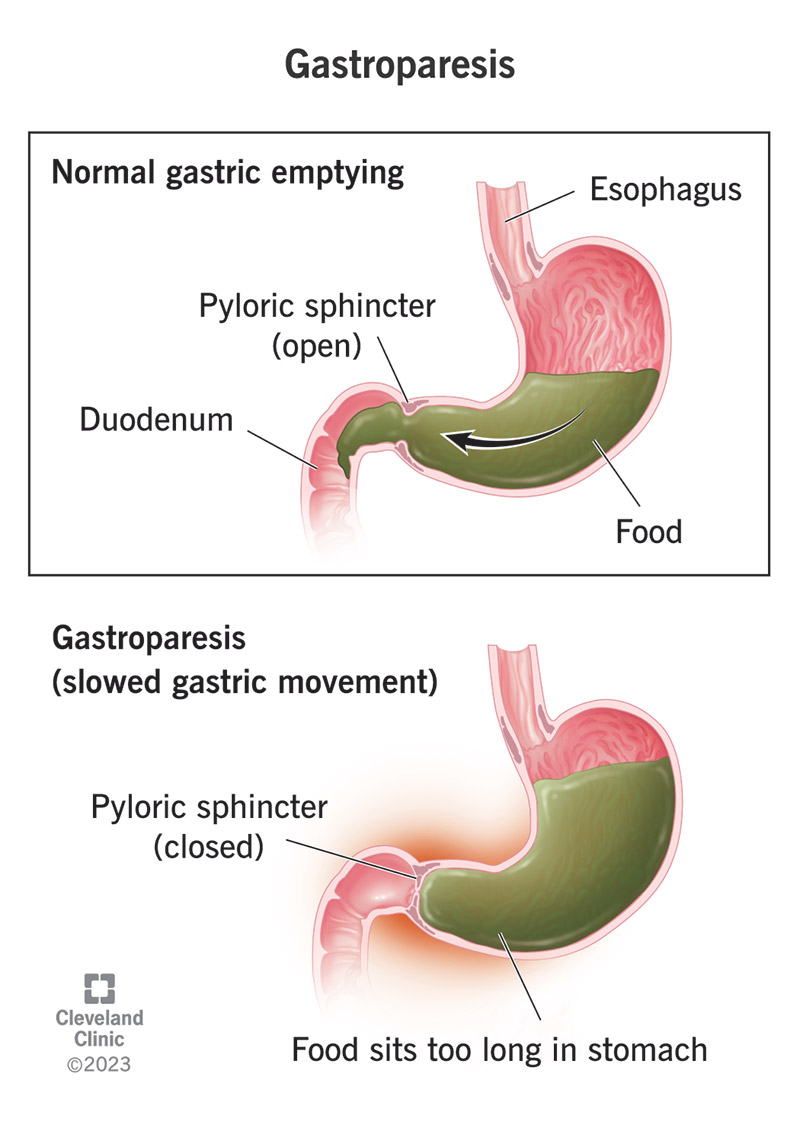
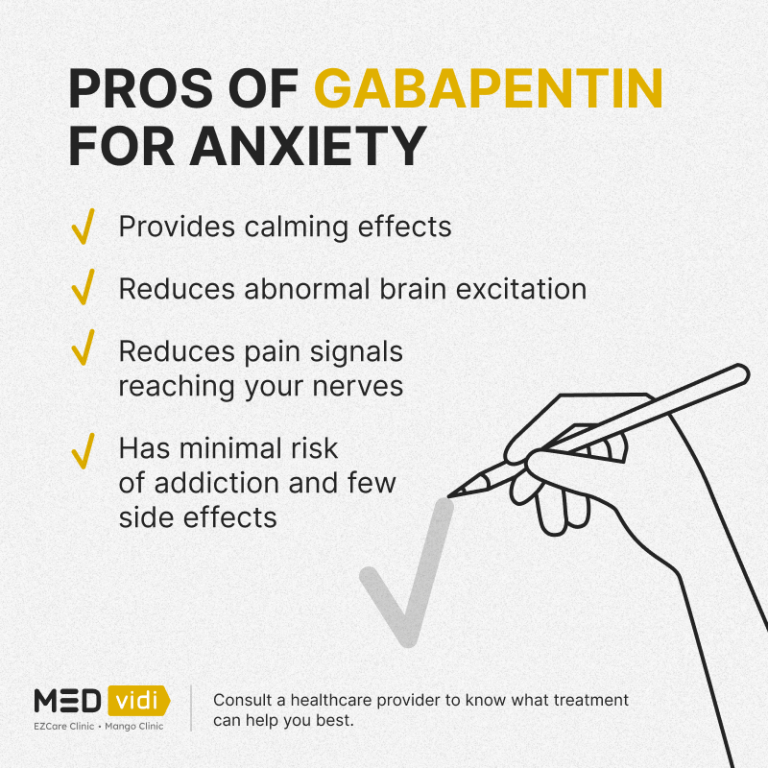
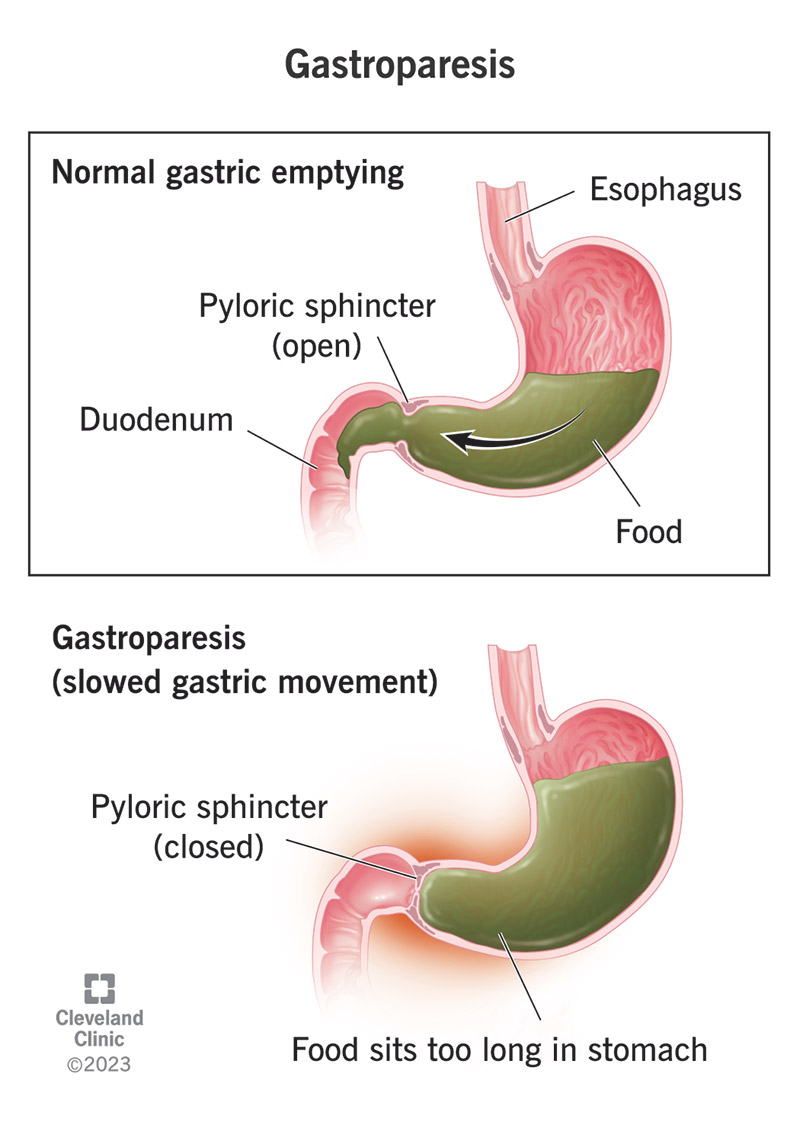
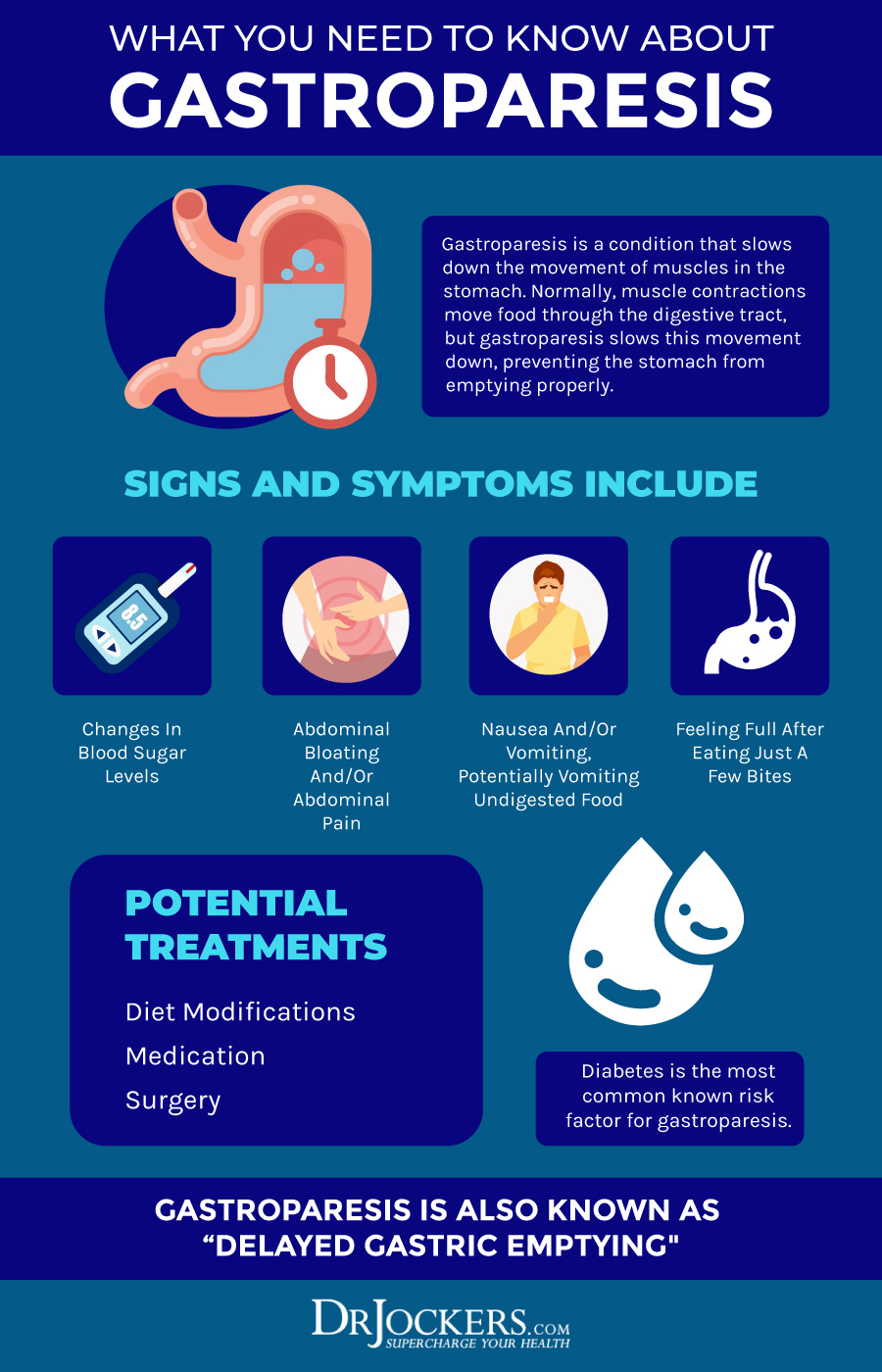
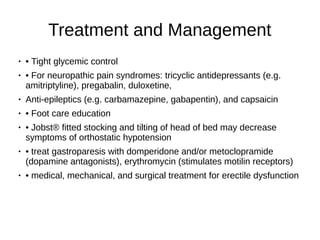
Several medications can delay gastric emptying and should be avoided with gastroparesis. However, most of the below-listed medications are vital to treat or prevent serious diseases. Don’t stop or change your medications without consulting your health care provider. Gastric peroral endoscopic pyloromyotomy therapy for refractory gastroparesis. Curr Treat Options Gastroenterol. 2017;15 (4):637-647. 41. Khoury T, Mizrahi M, Mahamid M, et al. State of the art review with literature summary on gastric peroral endoscopic pyloromyotomy for gastroparesis. J Gastroenterol Hepatol. 2018;33 (11):1829-1833. 42. Treatment Treating gastroparesis begins with finding and treating the condition that's causing it. If diabetes is causing your gastroparesis, your healthcare professional can work with you to help you control your blood sugar levels. In the first study of its kind, Massachusetts General Hospital researchers showed that low-dose gabapentin is an effective and well-tolerated treatment for patients presenting with functional dyspepsi Gabapentin: A Detailed Review of Effectiveness, Side Effects, and Comparisons for Treating Gastroparesis. In summary, gabapentin for the treatment of gastroparesis is an off-label medication, meaning it's not officially approved by the FDA for this condition. INTRODUCTION Gastroparesis is a syndrome of objectively delayed gastric emptying in the absence of a mechanical obstruction and cardinal symptoms of nausea, vomiting, early satiety, belching, bloating, and/or upper abdominal pain. This topic will review the treatment of gastroparesis. Differentiating between the etiologies of gastroparesis may allow developing strategies that could increase QOL in gastroparesis patients. For instance, it has been suggested that treatment for gastroparesis may produce different responses depending on whether gastroparesis occurs in diabetic or non-diabetic patients. I have gastroparesis and taking Gabapentin how long does it take to get used to symptoms especially fatigue? Do you eventually adjust? Gastroparesis can be a serious problem where the GI tract literally “slows down”. This issue is common in patients with diabetes. Bloating, abdomnial pain, nausea, vomiting, and a feeling of fullness are all possible symptoms of gastroparesis. There are also medications that can worsen gastroparesis. The case: KD is a 62 year old female who [] Gastroparesis (GP), a historically vexing disorder characterized by symptoms of nausea, vomiting, abdominal pain, early satiety, and/or bloating, in the setting of an objective delay in gastric emptying, is often difficult to treat and carries a Environmental hypersensitivity and anxiety and depression are among the factors that can cause this disease. In this regard, gabapentin as a gamma-aminobutyric acid (GABA) analog used in the treatment of neuropathic pain and may be effective in controlling the symptoms of GI disorders. Medication-induced gastroparesis is reversible, and discontinuing the medication is generally curative. This case report discusses 2 cases of medication-induced gastroparesis which were initially diagnosed as diabetic gastroparesis, and thorough history taking revealed the cause to be medication induced. Treatment of gastroparesis depends on the cause, the severity of symptoms and complications, and how well patients respond to different treatments. As a result, the main goals of treatment for gastroparesis are alleviation of symptoms, correction of malnutrition, and resumption of adequate oral intake of liquids and solids. 6. Clinicians should consider the use of neuromodulators to treat gastroparesis associated abdominal pain but should not use opioids. 7. Clinicians can consider gastric electrical stimulation for gastroparesis patients with refractory/intractable nausea and vomiting who have failed standard therapy and are not on opioids. 8. The authors concluded that gastroelectrical stimulation may be an effective therapy treatment in symptoms of gastroparesis with normal gastric emptying or rapid gastric emptying. Further studies on treating gastroparesis-like symptoms with non-delayed gastric emptying are needed. Gabapentin and Diabetic gastroparesis - a phase IV clinical study of FDA data Summary: Diabetic gastroparesis is reported as a side effect among people who take Gabapentin (gabapentin), especially for people who are female, 60+ old, also take Lantus, and have Gastroesophageal reflux disease. Currently, some doctors are prescribing the gabapentin to prevent migraine headaches, treat nystagmus, and reduce neuropathic pain. [5, 6, 7] However, there are few studies on analgesic effects of gabapentin and other effects of it. Abstract Gastroparesis is a gastrointestinal motility disorder characterized by nausea, vomiting, early satiation, postprandial fullness, bloating, and upper abdominal pain. The diagnosis requires documented delay in gastric emptying with an optimal test such as scintigraphy or stable isotope gastric emptying breath test in the absence of mechanical obstruction. The pathophysiologic mechanisms An accurate diagnosis is necessary to treating gastroparesis, since the treatment depends on the cause. If your doctor diagnosed an underlying disease or condition that is causing the gastroparesis, the treatment will focus on correcting or reversing that condition; if there is no underlying cause This guideline presents recommendations for the evaluation and management of patients with gastroparesis. Gastroparesis is identified in clinical practice through the recognition of the clinical symptoms and documentation of delayed gastric
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |