Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
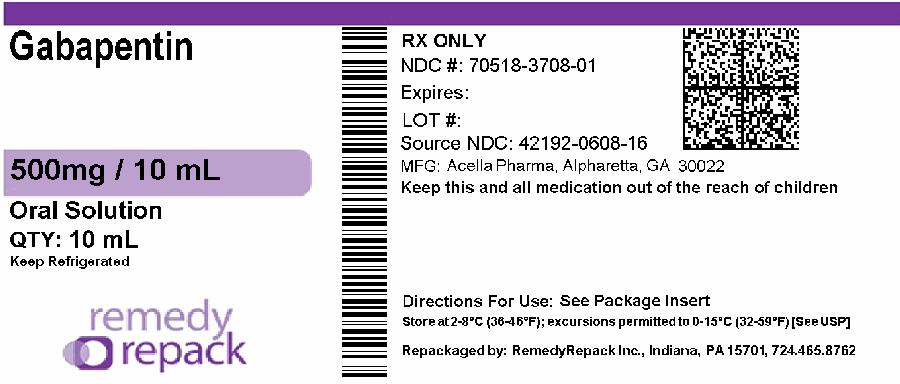
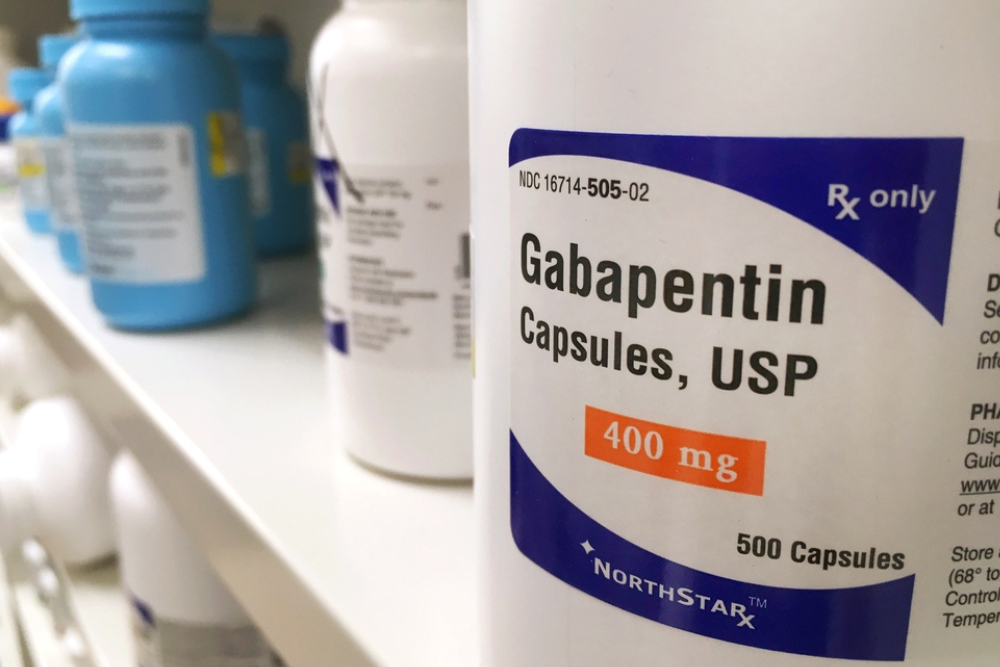
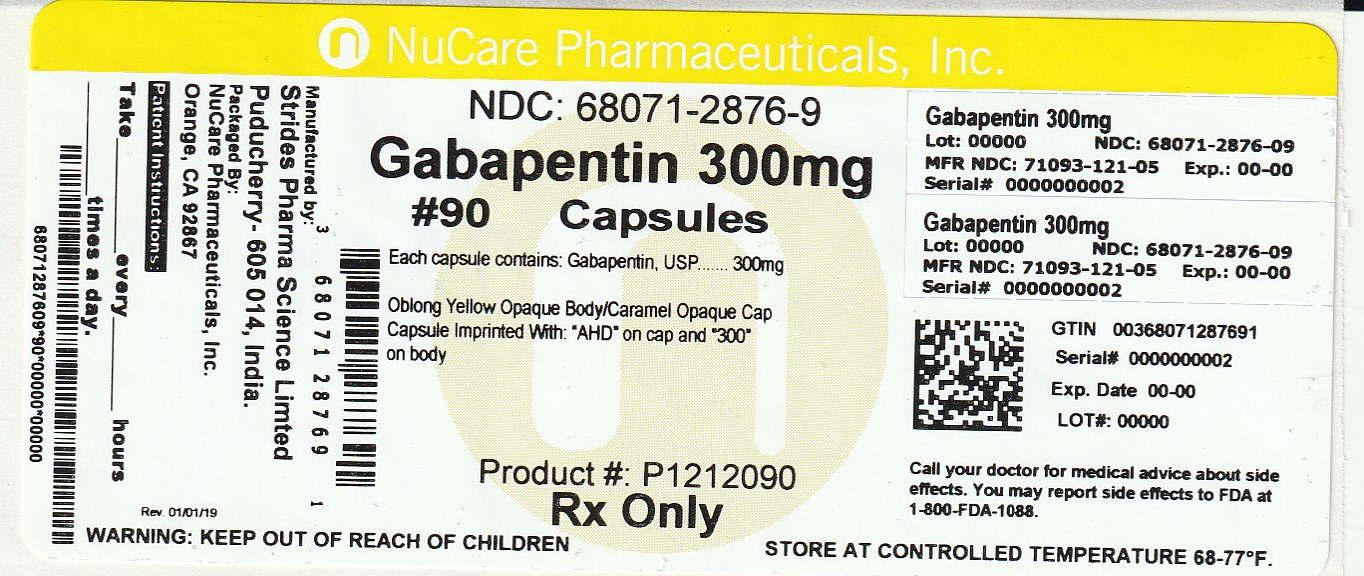
Patients dealing with diabetic neuropathy, post-herpetic neuralgia (pain after shingles), and other forms of nerve pain are often prescribed gabapentin. But like any medication, gabapentin doesn’t come without its potential side effects—and for some, it can feel like it’s making things worse instead of better. It can take one to two weeks to feel the full effects of Gabapentin for nerve pain. Some people use this medication long-term. Learn how long you should take Gabapentin for nerve pain. Gabapentin is also effective for the treatment of neuropathic pain. Neuropathic pain may respond to opioid analgesics. There is evidence of efficacy for tramadol hydrochloride, morphine, and oxycodone hydrochloride; however, treatment with morphine or oxycodone hydrochloride should be initiated only under specialist supervision. In the 2016 report, most of the available randomized control trial (RCT) data pertained to diabetic peripheral neuropathy (DPN) and post-herpetic neuralgia (PHN), it was concluded that for DPN there was greater reduction in neuropathic pain and increased risk of adverse events associated with gabapentin compared with placebo. PHARMACOLOGICAL OPTIONS FOR MANAGEMENT OF NEUROPATHIC PAIN Gabapentinoids – both pregabalin and gabapentin go through minimal first-pass metabolism and are eliminated unchanged in the urine. Renal impairment will consequently decrease gabapentinoids elimination and result in potential drug accumulation. It is a good practice to review (at least twice per annum) patients with declining kidney Compare risks and benefits of common medications used for Peripheral Neuropathy. Find the most popular drugs, view ratings and user reviews. Peripheral neuropathy is a painful condition deriving from many and varied etiologies. Certain medications have been implicated in the iatrogenic development of Drug Induced Peripheral Neuropathy (DIPN) and include chemotherapeutic agents, Gabapentin can help relieve nerve pain in some people with postherpetic neuralgia (nerve pain after shingles) and peripheral diabetic neuropathy (nerve pain in the feet in people with diabetes). Patients suitable for gabapentin should have a clear neuropathic pain syndrome, characterized by sharp, shooting, lancinating and/or burning pain, in a nerve root (radicular) or stocking/glove distribution. Adult dosing: Gabapentin is started at low doses (100 mg to 300 mg total daily) and increased by 100 – 300 mg every 1-3 days to effect. Millions of people suffer from the burning, tingling, and numbness of a form of neuropathy called idiopathic sensory polyneuropathy. A recent study directly comparing four medications produced disappointing results, but is a step in the right direction. Abstract Background: Drugs for neuropathic pain have incomplete efficacy and dose-limiting side-effects when given as monotherapy. We assessed the efficacy and tolerability of combined nortriptyline and gabapentin compared with each drug given alone. Gabapentin plus nortriptyline cuts neuropathic pain Neuropathic pain is relieved more effectively by combination treatment with the anticonvulsant gabapentin and the antidepressant nortriptyline than by treatment with either drug alone, a study published online in The Lancet has shown. Patients with diabetic neuropathy treated with gabapentin in combination with venlafaxine reported pain relief and improvements in quality of life compared to those in a placebo group and to those who received gabapentin and placebo [77]. Gabapentin and pregabalin are used mostly in the management of diabetes-induced peripheral neuropathy and postherpetic neuralgia. The analgesic effect of gabapentin arises from increased GABA synthesis, α2δ subunit binding of voltage-gated calcium channels, and non-NMDA receptor antagonism. A gastroretentive gabapentin formulation for the treatment of painful diabetic peripheral neuropathy: efficacy and tolerability in a double-blind, randomized, controlled clinical trial. View gabapentin information, including dose, uses, side-effects, renal impairment, pregnancy, breast feeding, monitoring requirements and important safety information. First-line drug therapy for painful diabetic peripheral neuropathy includes duloxetine, gabapentin, amitriptyline, and pregabalin; however, these medications do not restore sensation to affected extremities. Evidence for long-term benefit and safety of first-line treatment options is lacking. Key Messages Overall, evidence suggests that there is a greater reduction in neuropathic pain (NP) with gabapentin compared with placebo in adults who have a variety of conditions, including diabetic peripheral neuropathy and postherpetic neuralgia. For short-term treatment of painful diabetic neuropathy and postherpetic neuralgia, gabapentin may be as effective as tricyclic antidepressants Gabapentin at doses of 1800 mg to 3600 mg daily (1200 mg to 3600 mg gabapentin encarbil) can provide good levels of pain relief to some people with postherpetic neuralgia and peripheral diabetic neuropathy. Evidence for other types of neuropathic pain is very limited. The outcome of at least 50% pai The treatment of painful diabetic neuropathy (PDN) still remains an important unmet medical need. Low doses of trazodone added to full gabapentin dose recently demonstrated improvement in pain and sleep outcomes while being well tolerated in patients with PDN. This is a phase II, randomized, placebo-controlled, dose-finding study which aimed to assess the efficacy and safety of three different
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |