Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
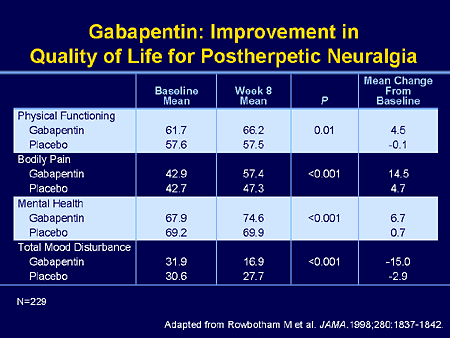
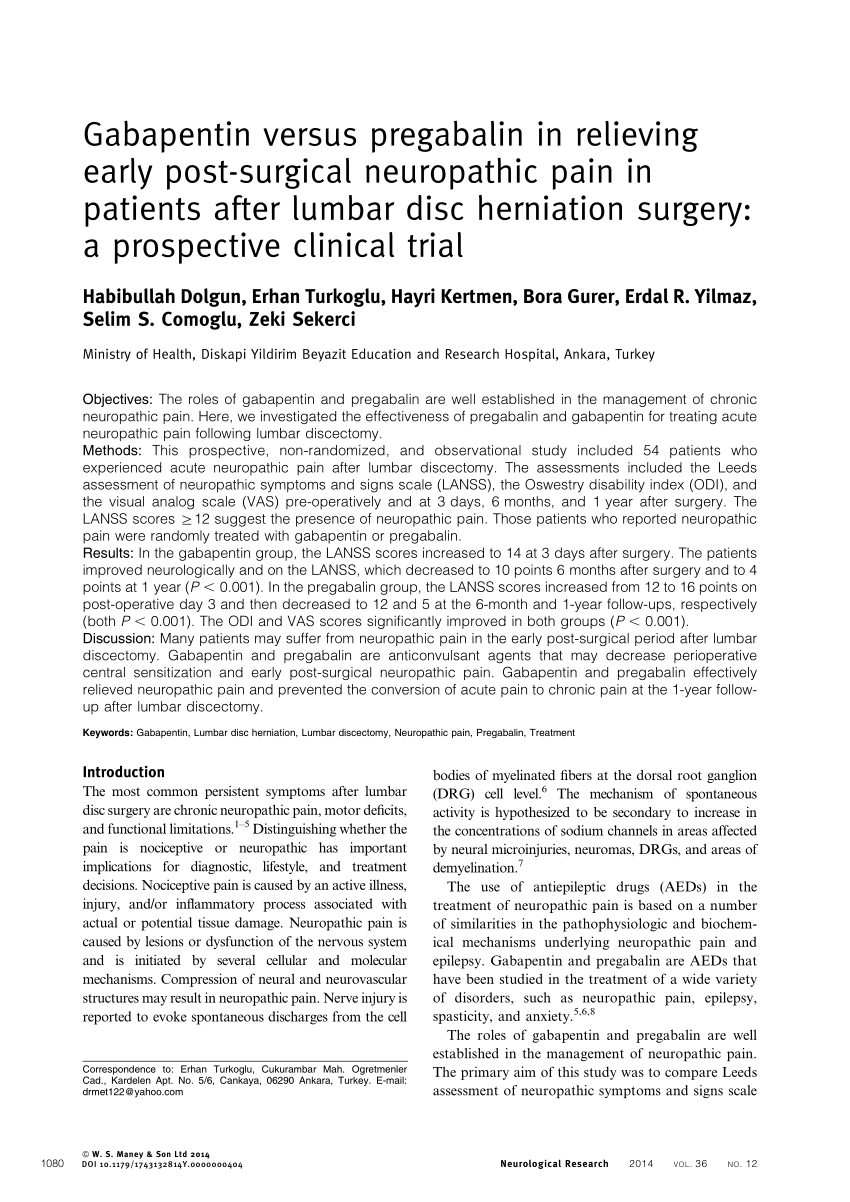
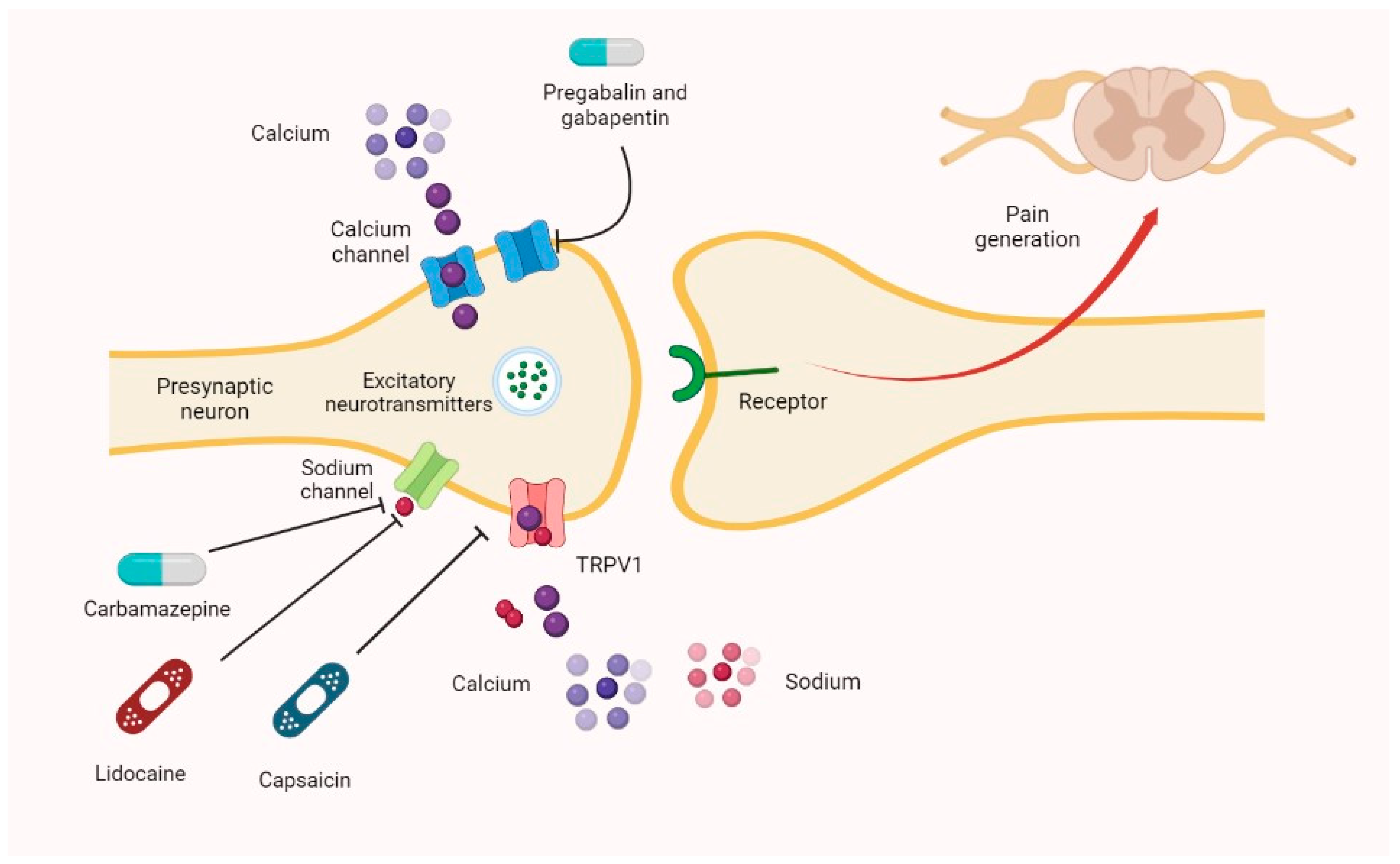
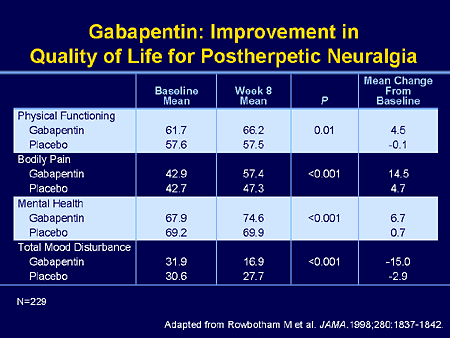
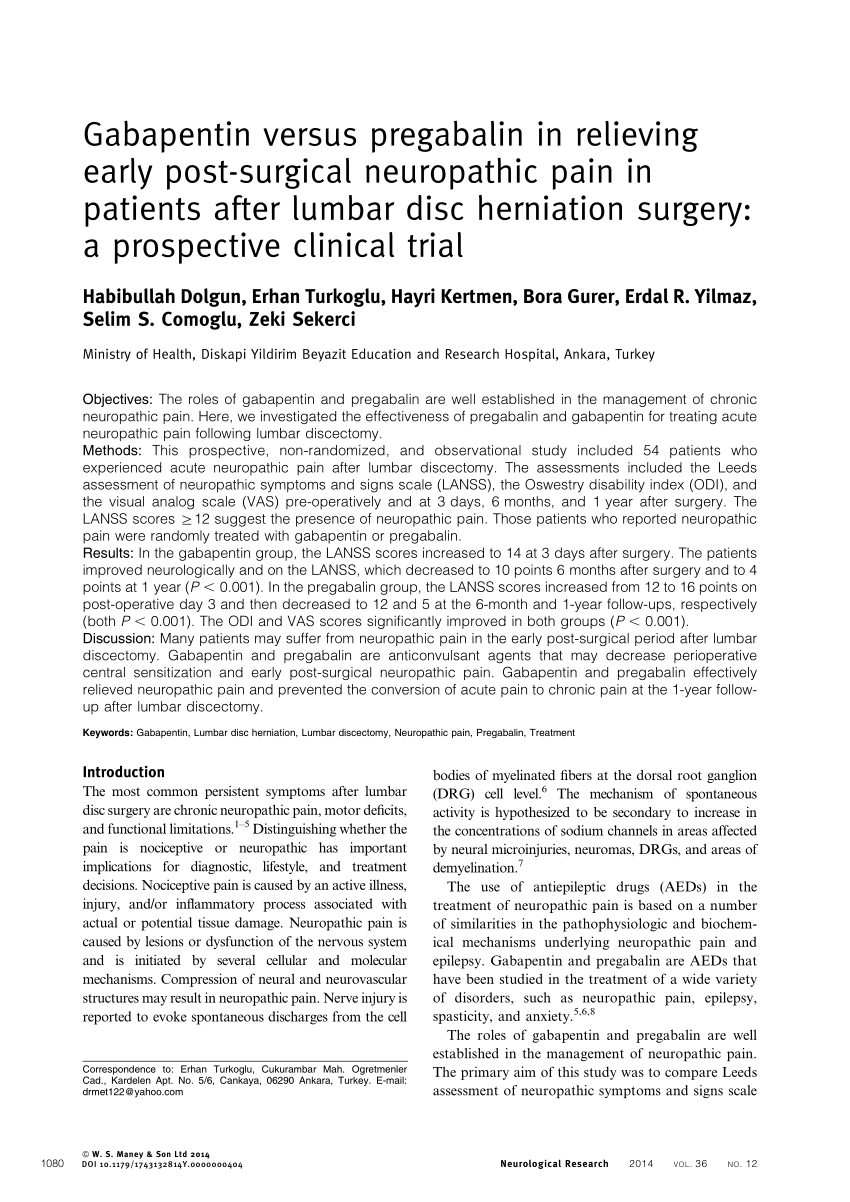
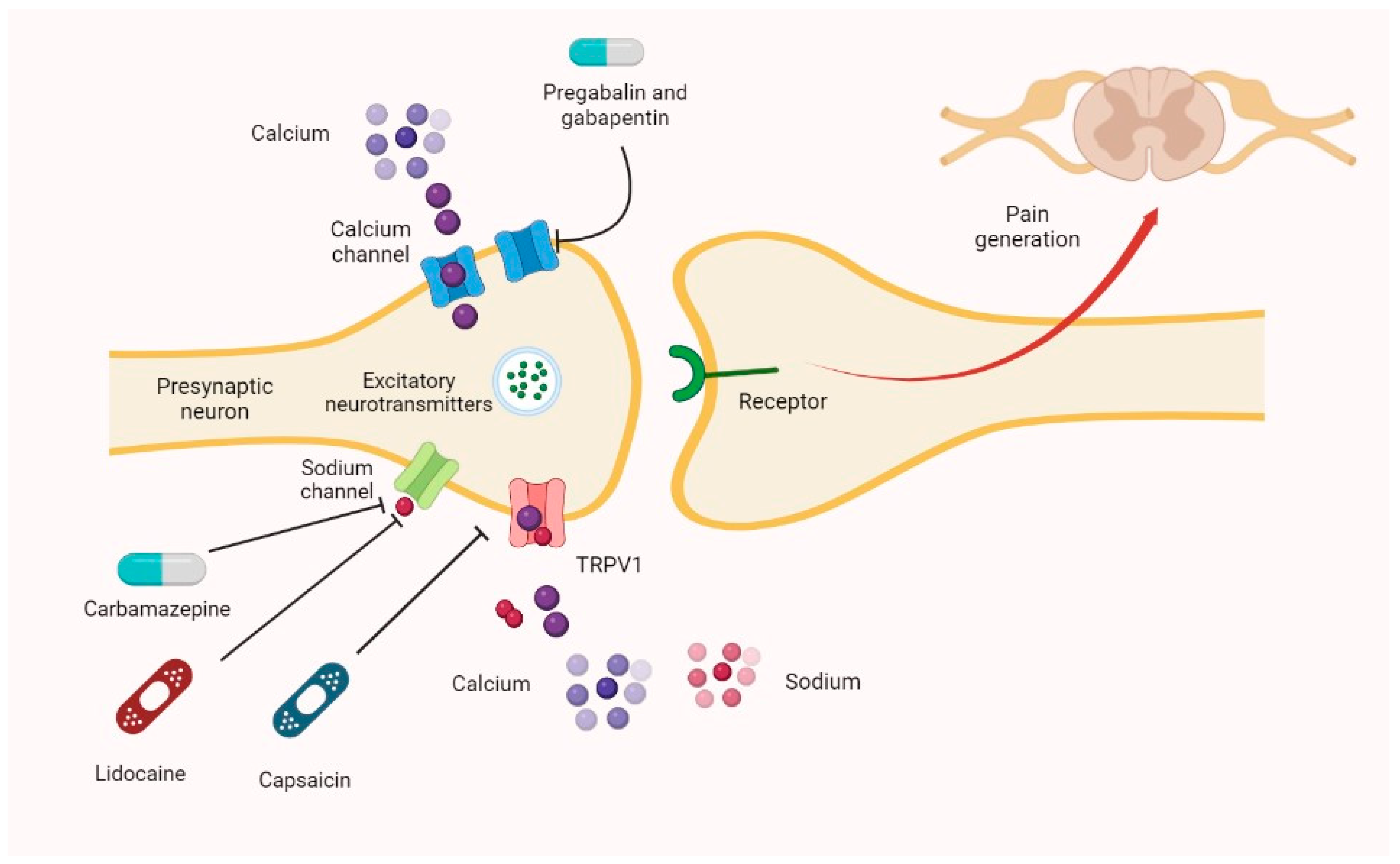
Pregabalin (Lyrica) and gabapentin (Neurontin) are both approved to treat nerve pain. How are they different, and which one is preferred? Compare both meds here. Introduction: Neuropathic pain is a prevalent and burdensome condition, and both pregabalin and gabapentin are widely used for its treatment. However, there is a lack of clarity regarding their comparative efficacy and safety. This meta-analysis aims to evaluate and compare the effectiveness and Neuropathic pain (NeP) affects 6–10% adults worldwide. It represents an even greater burden than non-neuropathic chronic pain, significantly impacting on patients' lives and with wider socio-economic consequences.1,2 I now advocate for deprescribing gabapentin when patients do not achieve adequate pain relief for chronic neuropathic pain at a cumulative daily dose of 1800 mg. Instead, I consider pregabalin as a substitute for gabapentin in patients with inadequate pain control rather than further dose escalations. Pregabalin and gabapentin are often considered first-line treatments for various neuropathic pain syndromes, generally irrespective of cause. Use of gabapentin for central neuropathic pain is therefore off-label. However, gabapentin is recommended by NICE as a first-line treatment option for adults with all types of neuropathic pain (except trigeminal neuralgia). Interactions There are no clinically relevant pharmacokinetic interactions between gabapentin and pregabalin. Pregabalin and gabapentin can be effective as first line treatment for some people with neuropathic pain such as post-herpetic neuralgia and diabetic peripheral neuropathy They are not effective for low back pain, sciatica, spinal stenosis, or episodic migraine, and their off-label use for these Abstract Pregabalin is an antagonist of voltage gated Ca2+ channels and specifically binds to alpha-2-delta subunit to produce antiepileptic and analgesic actions. It successfully alleviates the symptoms of various types of neuropathic pain and presents itself as a first line therapeutic agent with remarkable safety and efficacy. Preclinical studies in various animal models of neuropathic pain Neuropathic pain is a complex and often debilitating condition that affects millions of people worldwide. For those struggling to manage this type of pain, medications like Pregabalin and Gabapentin are frequently prescribed to provide relief. Pregabalin is approved for additional uses, including fibromyalgia and nerve pain in certain adults. Healthcare providers commonly prescribe these medications for off-label uses (non-FDA-approved uses) as well, such as anxiety disorders. Abstract Gabapentin (Neurontin 1 ) and pregabalin (Lyrica 2 ) are first- and second-generation α2δ ligands, respectively, and are both approved for use as adjunctive therapy in pain control. Although they do not bind to gamma-aminobutyric acid (GABA) receptors they have been successfully used to treat neuropathic pain conditions. Their mechanism of action is not yet fully understood, but ABSTRACT Pregabalin is one of the first-line treatments approved for the management of neuropathic pain (NeP). While many patients benefit from treatment with pregabalin, they are often treated with suboptimal doses, possibly due to unfamiliarity around prescribing the drug and/or side effects that can occur with up-titration. This narrative review discusses key aspects of initiating Can I prescribe gabapentin and pregabalin together for neuropathic pain? A clinical pharmacist walks through how to limit side effects while optimizing pain control. Neuropathic pain after spinal cord injury (SCI) has a significant negative impact on the patients’ quality of life. The objective of this systematic review is to examine the safety and efficacy of pregabalin (PGB) and gabapentin (GBP) in the Neuropathic pain is a prevalent and burdensome condition, and both pregabalin and gabapentin are widely used for its treatment. However, there is a lack of clarity regarding their comparative efficacy and safety. This meta-analysis aims to evaluate Pregabalin resulted in lower opioid consumption (OR 0.50, 95% CI 0.33-0.76). Gabapentin had a higher incidence of nausea and vomiting. Sensitivity analysis supported the efficacy of pregabalin. Conclusion: In conclusion, pregabalin demonstrated superior and faster efficacy in alleviating neuropathic pain than gabapentin did. Compared with gabapentin, pregabalin was more efficacious and safer for the treatment of neuropathic pain, with significant reductions in pain intensity and duration, opioid use, and adverse events. In a partial spinal nerve injury model, combination therapy with subeffective doses of gabapentin and pregabalin potentiated the therapeutic efficacy of spinal cord stimulation, a tool used for neuropathic pain relief, as evaluated via the von Frey test [119]. Gabapentin vs Pregabalin: Understanding the Differences Gabapentin and pregabalin are antiepileptic drugs commonly used for neuropathic pain management and pain reduction in adults. Both medications are classified as antiepileptic medications, but they have differences in pharmacokinetics, safety profile, and clinical applications. This article explores their efficacy, dosing, safety of Neuropathic pain largely influences the well-being of patients. Anticonvulsant and antidepressant medications, such as Pregabalin, Gabapentin, and Amitriptyline, are routinely prescribed as initial treatments for neuropathic pain. The study sample
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |