Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
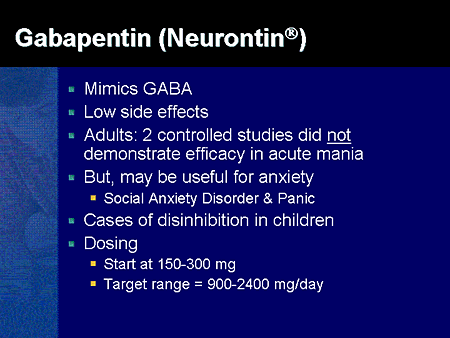
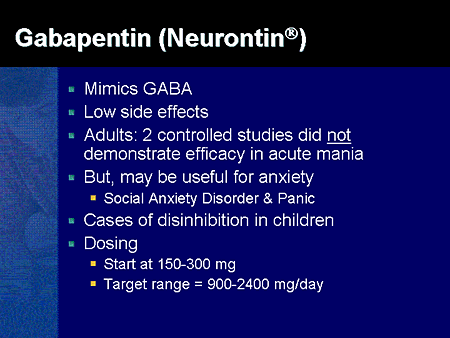
The inclusion criteria of the RCTs were patients >18 years, patient undergoing inpatient surgeries (open or laparoscopic) under general anesthesia, preoperative administration of gabapentin irrespective of dose and duration before surgery (compared to a placebo), and trials reporting opioid consumption as the primary outcome. In this cohort study, perioperative gabapentin use was associated with increased risk of delirium, new antipsychotic use, and pneumonia among older patients after major surgery. These results suggest careful risk-benefit assessment before prescribing gabapentin for perioperative pain management. Abstract Purpose of review: This review summarizes the risks and benefits of gabapentinoids (gabapentin and pregabalin) for perioperative pain control and the controversies surrounding their use in a variety of settings. We review current literature with the goal of providing patient-centric and procedure-specific recommendations for the use of these medications. This cohort study examines whether perioperative gabapentin use among older adults after major surgery is associated with in-hospital adverse clinical events. You will need to temporarily stop taking the following medications before your surgery. These medications can thin your blood, change its clotting, and slow the healing process after surgery. To ensure a successful hip replacement surgery, it is crucial to stop taking certain medications 1 week before surgery or as directed by your healthcare provider. On the day of surgery, gabapentin was administered orally 2 h before the procedure—400 mg for Group A and 800 mg for Group B. A fellow anesthesiologist administered the medication to maintain double-blinding, ensuring that study participants and researchers remained unaware of their group allocations. St. John’s wart (please do not take 14 days prior to surgery), Vitamin E, Multi-Vitamins if it also contains Vitamin E If you are having a cervical or lumbar spinal fusion surgery you will not be able to take NSAIDS or medications containing Aspirin for about 3 months (until your doctor tells you that your fusion appears solid). For individuals preparing for surgery, managing pain effectively can be crucial for recovery. However, the use of Gabapentin before surgical procedures raises questions about its safety and efficacy in that context. The primary concerns revolve around potential interactions with anesthesia and other medications administered during surgery. Conclusion Gabapentin (1200 mg) administered orally 2 h before surgery decreased the intraoperative fentanyl and isoflurane consumption, postoperative analgesic requirements, postoperative pain, and the incidence of postoperative nausea and vomiting, but increased dizziness. We need to unwind the automaticity of gabapentin use in the perioperative period. For example, in this study, 5 80% of gabapentin users received gabapentin on the day of surgery, suggesting that it was started prior to any patient report of pain, representing an opportunity to de-escalate gabapentin use for some patients. On the day of surgery, patients were assigned randomly, in a double-blind fashion, via a random-number table to receive 1200 mg gabapentin (Gabapentin) or an identical-looking placebo (Control) orally 1-2 hours before surgery (n = 20 per group). Personnel involved in patient management and data collection were unaware of the group assignment. Prescription of gabapentin and pregabalin in the perioperative period has become increasingly common, if not de rigueur. These gabapentinoids have become ubiquitous components of protocols for early recovery after surgery and multi-modal analgesia. Neither is approved by the US Food and Drug Administration (FDA) for preventing or treating surgical pain, but their use is predicated on Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Gabapentin, an anticonvulsant, recently has been suggested as an effective post-operative “analgesic” agent. The objective of the present study was to examine the analgesic effectiveness and opioid-sparing effects associated with the use of a single Conclusion: Gabapentin 600 mg administered 1 hr before laparoscopic abdominal surgery is as effective as gabapentin 900 mg for PONV control and VAS reduction of 24-hour postoperative pain scores with fewer side effects. On the other hand, gabapentin 300 mg did not demonstrate good control of PONV, or pain control compared to higher doses. This cohort study examines whether perioperative gabapentin use among older adults after major surgery is associated with in-hospital adverse clinical events. This randomized clinical trial investigates the effect of perioperative gabapentin treatment vs placebo on postsurgical pain in patients undergoing head and neck mucosal surgery. The most common dose of gabapentin assessed was 1200 mg daily (12 studies), with some studies using doses as low as 300 mg daily (Table 1). Eleven studies (25, 28 – 33, 36, 38 – 40) administered gabapentin as a single dose within 1 h to 2 h before surgery; the remainder involved initiating therapy on the day before surgery or continuing it for up to 10 days after surgery (Table 1). With Consider the following when using gabapentinoids in the perioperative period The evidence supports the use of gabapentinoids in the perioperative period. A typical dose range for perioperative gabapentin is 200-300 mg and 25-50 mg for pregabalin. Given the opioid-sparing effect of gabapentinoids, lower doses of perioperative narcotics may be used.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |