Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
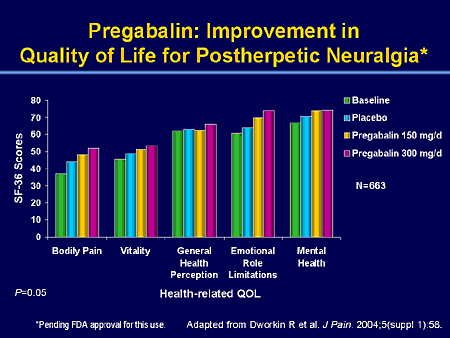
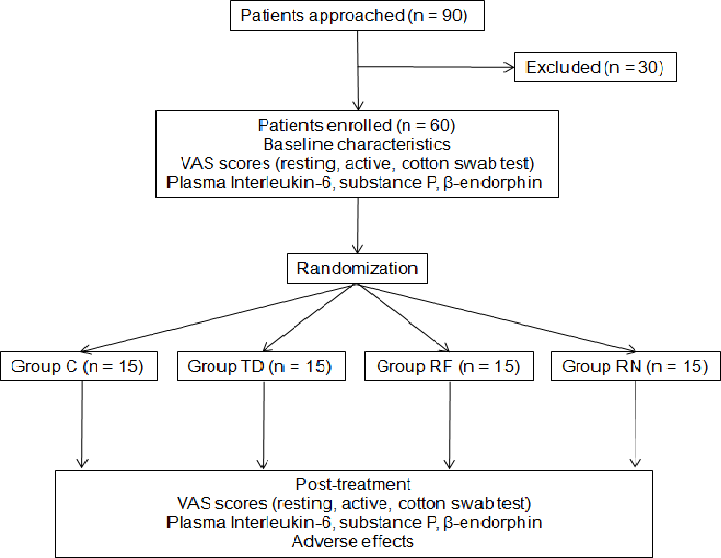
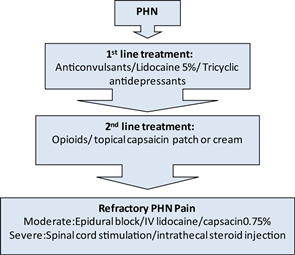
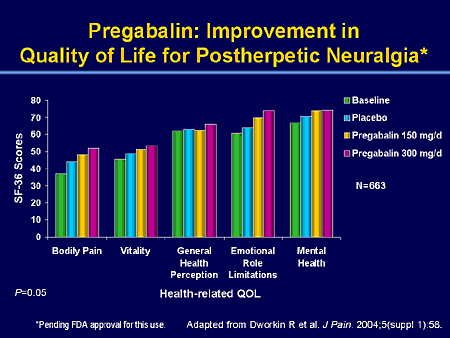
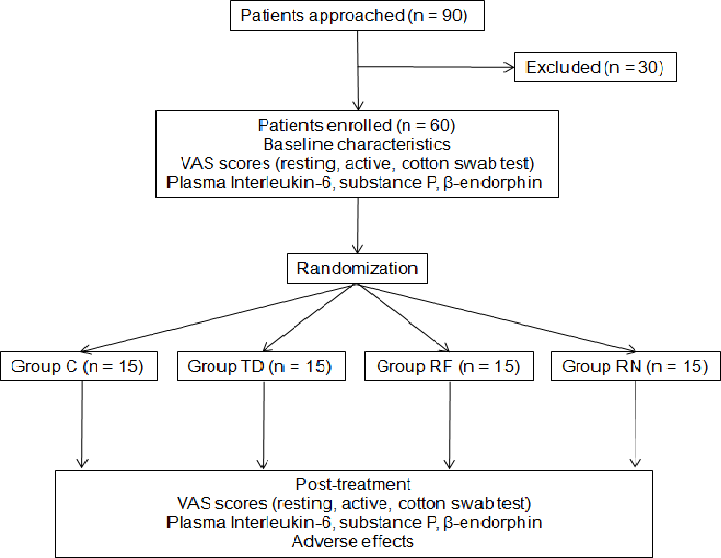
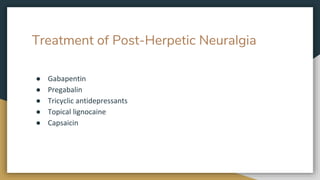
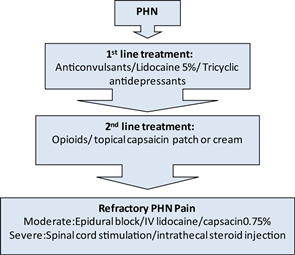
Abstract Although both gabapentin and pregabalin are first-line drugs for neuropathic pain including postherpetic neuralgia (PHN), no report has directly compared the magnitude of pain relief and the incidence of side effects of both drugs. By substituting gabapentin with pregabalin in postherpetic neuralgia therapy, we can compare the two drugs. Therapy with pregabalin is better compared to amitriptyline in postherpetic neuralgia patients, however, a similar study in a larger sample is required to validate the present findings. Abstract Background: Both gabapentin and pregabalin are approved for the management of postherpetic neuralgia (PHN), although dosing and pharmacokinetic differences between these medications may affect their use in actual practice. Accumulation can cause renal failure resulting in adverse effects. Formulations Gabapentin is available in two extended-release formulations in addition to the immediate release: a gastric retentive formulation (GBP-GR) and a gastro-retentive prodrug gabapentin enacarbil that are approved for the management of postherpetic neuralgia. Keywords: Peripheral neuropathic pain, Post-herpetic neuralgia, Diabetic neuropathy, Pregabalin, Gabapentin, Cost-effectiveness analysis Background Neuropathic pain (NeP) is defined by the International Association for the Study of Pain (IASP) as “Pain caused by a lesion or disease of the somatosensory nervous system”. Aims/Background Postherpetic neuralgia (PHN) is a common chronic pain disease that persists after the rash (clusters of clear blisters on the surface of the skin) has healed, adversely affecting the quality of life of affected patients. Gabapentin (GPT) and pregabalin (PGB) are two commonly used drugs for the treatment of PHN, but there have been broad concerns regarding their efficacy and We conducted a retrospective analysis of medical records of PHN patients who received combination therapy with gabapentin and pregabalin at our hospital. Data collected included numeric rating scale (NRS) pain scores before and after combination therapy, as well as the duration of each therapy. Statistical analysis was performed using SPSS Request PDF | Replacement of Gabapentin with Pregabalin in Postherpetic Neuralgia Therapy | Although both gabapentin and pregabalin are first-line drugs for neuropathic pain including postherpetic By substituting gabapentin with pregabalin in postherpetic neuralgia therapy, we can compare the two drugs. Methods. In 32 PHN patients being administered gabapentin, without changing the frequency of dosing, the drug was substituted with pregabalin at one-sixth dosage of gabapentin. Abstract Objective: To determine the utility of substitution of pregabalin (PGB) for gabapentin (GBP) therapy in the relief of neuropathic pain (NeP) in patients with peripheral neuropathy (PN). The study aims to systematically evaluate the clinical effect of gabapentin in the treatment of postherpetic neuralgia (PHN). Data were retrieved electronically from PubMed, Embase, CNKI, the China Biomedical Database, and the Library of Clinical Database, By substituting gabapentin with pregabalin in postherpetic neuralgia therapy, we can compare the two drugs. Methods: In 32 PHN patients being administered gabapentin, without changing the frequency of dosing, the drug was substituted with pregabalin at one-sixth dosage of gabapentin. Abstract Aims/Background Postherpetic neuralgia (PHN) is a common chronic pain disease that persists after the rash (clusters of clear blisters on the surface of the skin) has healed, adversely affecting the quality of life of affected patients. Gabapentin (GPT) and pregabalin (PGB) are two commonly used drugs for the treatment of PHN, but there have been broad concerns regarding their By substituting gabapentin with pregabalin in postherpetic neuralgia therapy, we can compare the two drugs. Methods. In 32 PHN patients being administered gabapentin, without changing the frequency of dosing, the drug was substituted with pregabalin at one-sixth dosage of gabapentin. Replacement of gabapentin with pregabalin in postherpetic neuralgia therapy.(English) 1 reference stated in 21692969 10 September 2017 main subject gabapentin 0 references author name string Masataka Ifuku series ordinal 1 1 reference stated in 21692969 10 September 2017 Masako Iseki series ordinal 2 1 reference stated in Europe PubMed Central Purpose. Although both gabapentin and pregabalin are first‐line drugs for neuropathic pain including postherpetic neuralgia (PHN), no report has directly compared the magnitude of pain relief and the incidence of side effects of both drugs. By substituting gabapentin with pregabalin in postherpetic neuralgia therapy, we can compare the two drugs. Methods. In 32 PHN patients being Although both gabapentin and pregabalin are first-line drugs for neuropathic pain including postherpetic neuralgia (PHN), no report has directly compared the magnitude of pain relief and the inci This meta-analysis evaluated the clinical efficacy of pregabalin and gabapentin in the treatment of postherpetic neuralgia. Pregabalin was found to have a better overall therapeutic effect than gabapentin for patients with PHN. However, gabapentin was found to have a lower incidence of adverse reactions and a better safety profile. Further high-quality RCTs are needed to confirm the advantages By substituting gabapentin with pregabalin in postherpetic neuralgia therapy, we can compare the two drugs. Methods In 32 PHN patients being administered gabapentin, without changing the frequency of dosing, the drug was substituted with pregabalin at one-sixth dosage of gabapentin. The conversion ratio used in one study was “of the author’s creation”3 and in another study the authors assumed that pregabalin had six times greater pharmacological effect against neuropathic pain than gabapentin based on the maximum dose of each medicine.8 Bock-brader et al5 derived a potency ratio from EC50 data in post-herpetic
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |