Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 | 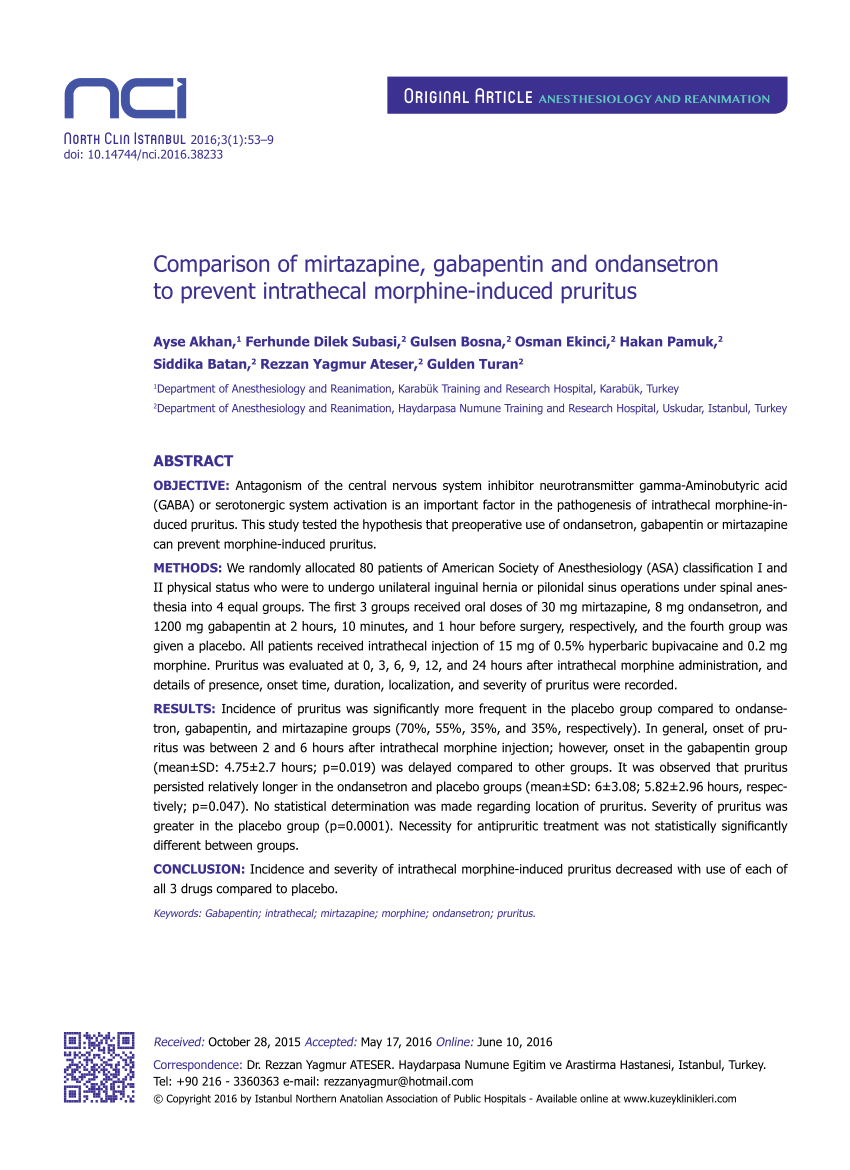 |
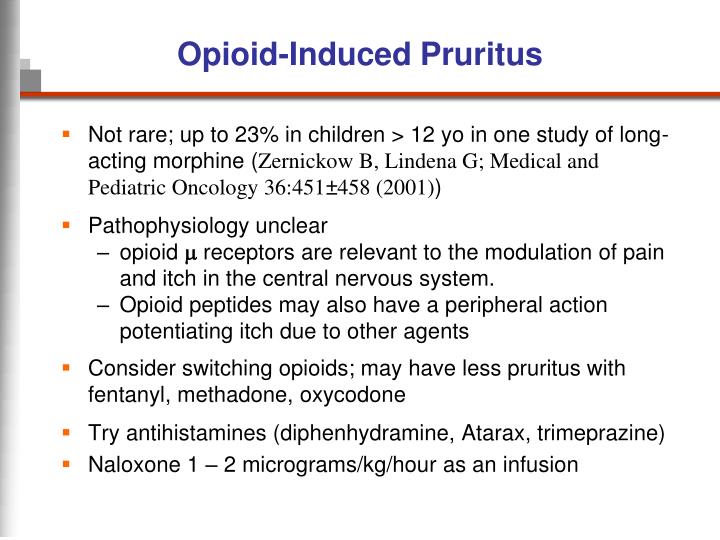
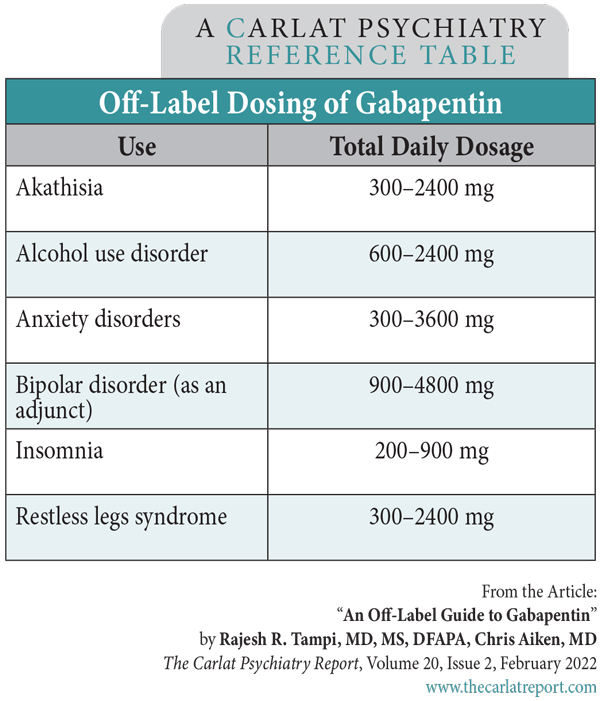
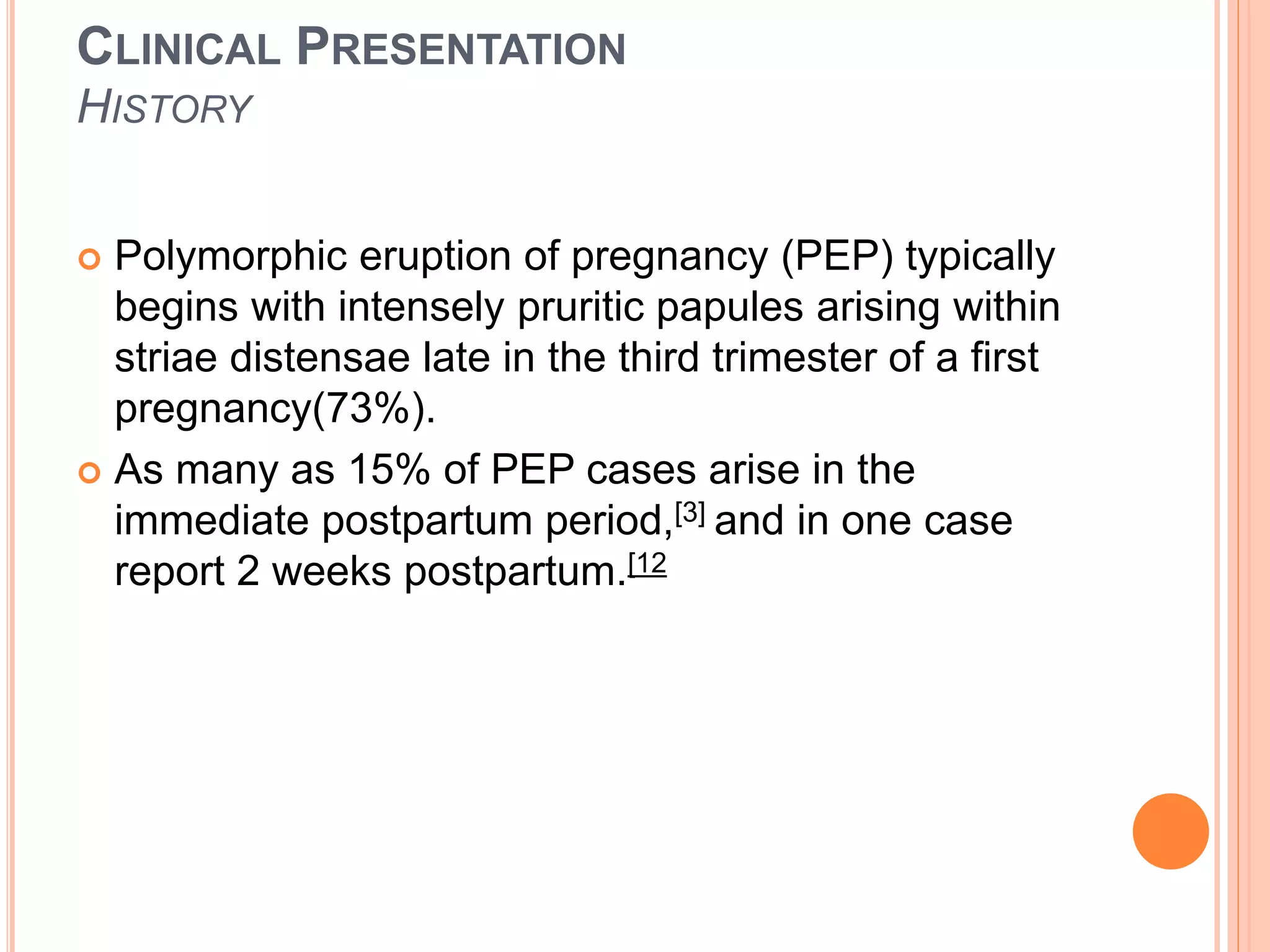
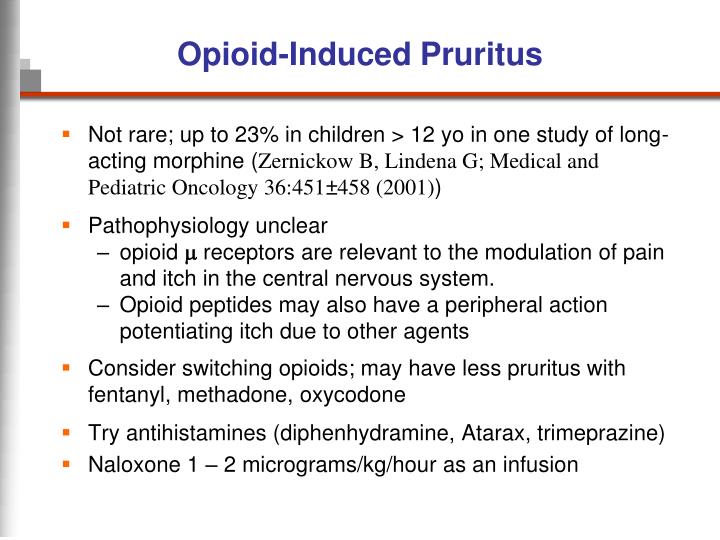
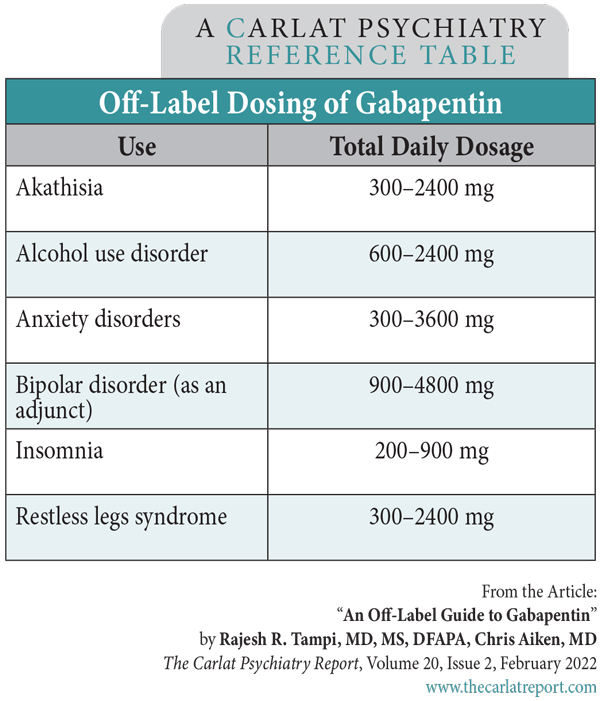
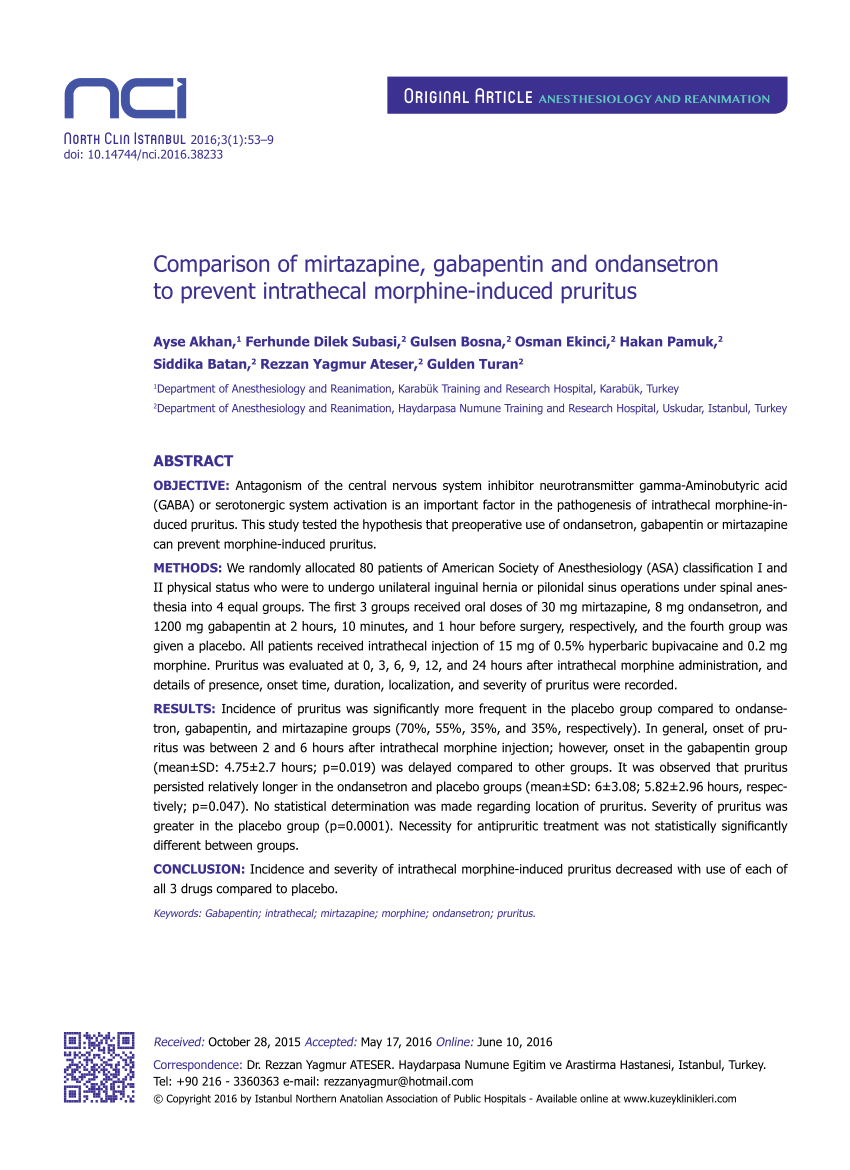
What is drug-induced pruritus? Pruritus is the medical name for itching. Drug-induced pruritus is an itch caused or triggered by medication. There are various itchy drug eruptions, but generally, the term ‘drug-induced pruritus’ implies that no primary rash is present — just scratch marks. Pruritus can begin within hours or up to several weeks after the drug responsible has first been The literature demonstrates gabapentin as an effective treatment modality in 11 articles for uremic pruritus, 9 articles for opioid-induced pruritus, and 2 articles for post-burn pruritus. Herein, the use of gabapentin and pregabalin, 2 medications well known for treating neuropathic pain and epilepsy that are occasionally used for relieving chronic pruritus is explored. The findings from original sources published to date to evaluate the use of gabapentin and pregabalin as antipruritic agents are explored. The successful utilization of gabapentin in alleviating pruritus in 3 patients with SCARs suggests a safe and effective treatment option. However, it is worth noting that gabapentin is renally cleared; thus, when employed for the management of SCARs with potential renal involvement (eg, drug reaction with eosinophilia and systemic symptoms The novel antiepileptic drugs pregabalin and gabapentin demonstrated significant therapeutic value in the treatment of pruritus, with a favorable safety profile. Generalized pruritus (without skin inflammation) is defined as the presence of itch over a wide area, and not localized to a specific part of the body. This entity includes idiopathic pruritus, pruritus in the elderly, symptomatic pruritus, pregnancy-associated pruritus, drug-induced pruritus, and psychogenic pruritus. Incidence and severity of intrathecal morphine-induced pruritus decreased with use of each of all 3 drugs compared to placebo. Keywords: Gabapentin, intrathecal, mirtazapine, morphine, ondansetron, pruritus Intrathecal use of morphine provides intense, prolonged analgesic effect, and it is frequently used in the relief of postoperative pain [1]. Uremic pruritus is one of the most prevalent and bothersome dermatologic symptoms in patients with end-stage renal disease. Some studies suggest a possible neuropathic cause of uremic pruritus. Gabapentin, an anticonvulsant, may control pruritus with neuropathic origin. The objectives of this study Limited data existed on the efficacy and safety of novel antiepileptic drugs (pregabalin and gabapentin) in treating pruritus. Overall gabapentin was an effective treatment for uremic, opioid induced, and post-burn pruritus in comparison to traditional antihistamines and placebo. Chronic pruritus is a distressing symptom that is often refractory to treatment. Patients frequently fail topical therapies and oral over-the-counter antihistamines, prompting the clinician to consider alternative therapies such as neuroactive agents. Herein, the use of gabapentin and pregabalin, 2 medications well known for treating neuropathic pain and epilepsy that are occasionally used for Herein, the use of gabapentin and pregabalin, 2 medications well known for treating neuropathic pain and epilepsy that are occasionally used for relieving chronic pruritus is explored. The findings from original sources published to date to evaluate the use of gabapentin and pregabalin as antipruritic agents are explored. Approximately 15% of people with chronic pruritus have other causes including systemic diseases with secondary itch, such as uremic pruritus and cholestatic pruritus, medication-induced pruritus such as pruritus due to immunotherapy, and infectious etiologies such as tinea corporis and scabies. The patients were started on oral gabapentin with an initial dose of 100 mg daily at bedtime, with the option to increase the dose by 100 mg daily per week up to 300 mg daily based on patient symptomatology. If scalp pruritus persisted at the 3-6 months follow-up, the dose was further increased by the prescribing physician (MMS). Conclusion The novel antiepileptic drugs pregabalin and gabapentin demonstrated significant therapeutic value in the treatment of pruritus, with a favorable safety profile. Compared to commonly used pruritus treatments such as antihistamines and antidepressants, these medications offered a promising alternative. This study tested the hypothesis that preoperative use of ondansetron, gabapentin or mirtazapine can prevent morphine-induced pruritus. There is currently no standardized algorithm for the treatment of chronic pruritus (CP), or itch lasting more than 6 weeks, in adults aged ≥ 65 years. The antiepileptic agents gabapentin and pregabalin, however, are gaining popularity in the The primary aim of this review was to evaluate the safety and efficacy of gabapentinoid use for CP in older adults, and to provide recommendations for gabapentin and pregabalin use in this patient population. On 10 November 2020, we conducted a search of the PubMed/MEDLINE databases using the search terms “gabapentin chronic pruritus,” “gabapentin itch,” “pregabalin chronic pruritus The use of gabapentin was responsible for a significant improvement in pruritus (p=0.0020). Besides itching and hyperchromic stain on the back, patients reported paresthesia and back pain. Generalized pruritus is a distressing symptom that can occur in several dermatologic and systemic disorders. 1 Generalized pruritus of unknown origin is that which affects patients without any underlying dermatologic or systemic disorder and is unassociated with rash. It most commonly occurs in older patients and persists for long periods, from months to years. In many cases, the itching may
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |